A Call to Reduce Mohs Skin Cancer Surgery: Doctors Respond to Peer Letters
Skin cancer treatment and surgery options vary widely. Even within one method, patients’ needs and surgeons’ choices differ. A recent study concluded too many stages of expensive surgery were being carried out within one type of treatment (Mohs Surgery) and used “Dear Colleague" performance evaluation letters in an effort to reduce these surgery stages, along with the related costs.
What is Mohs Surgery?
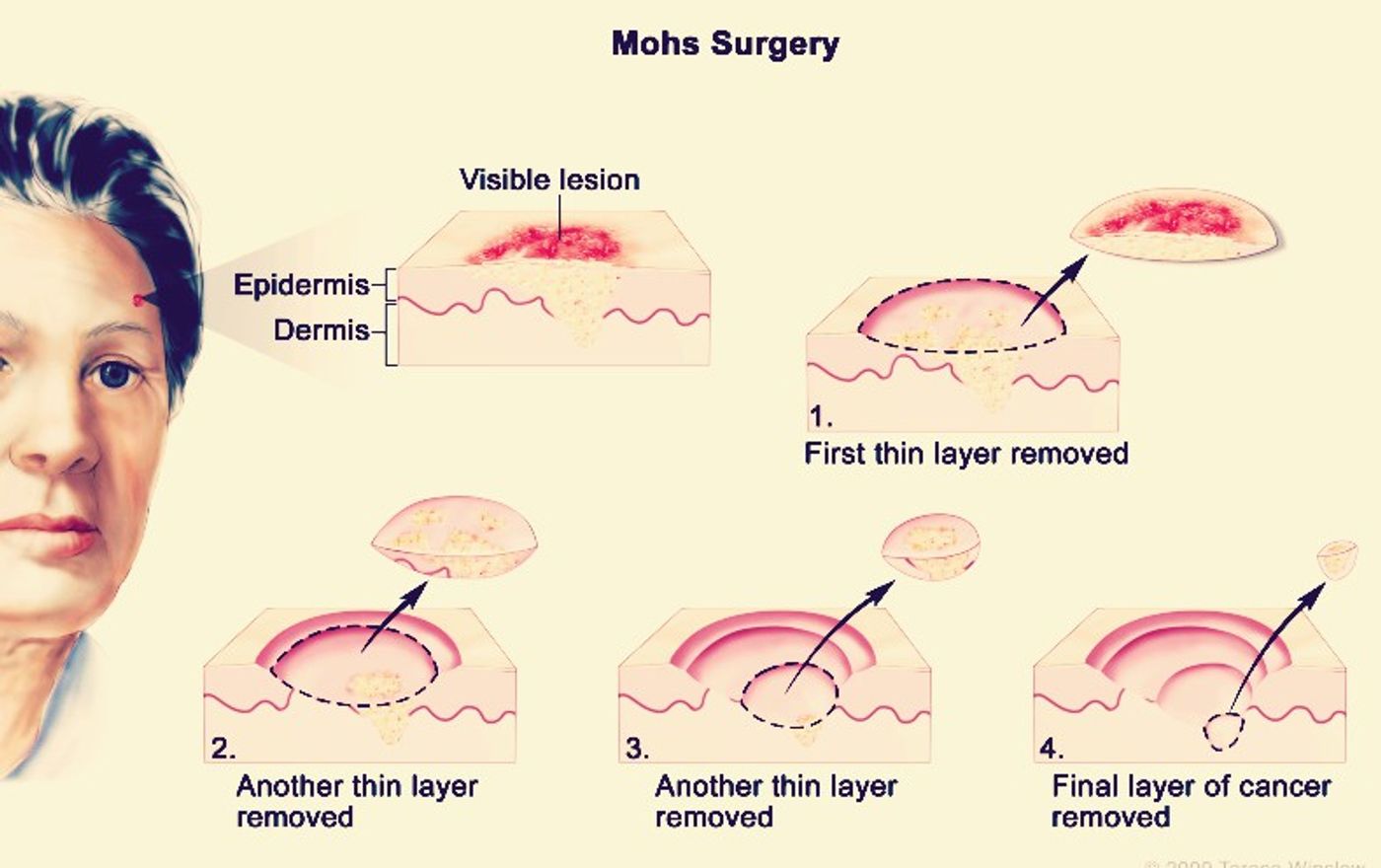
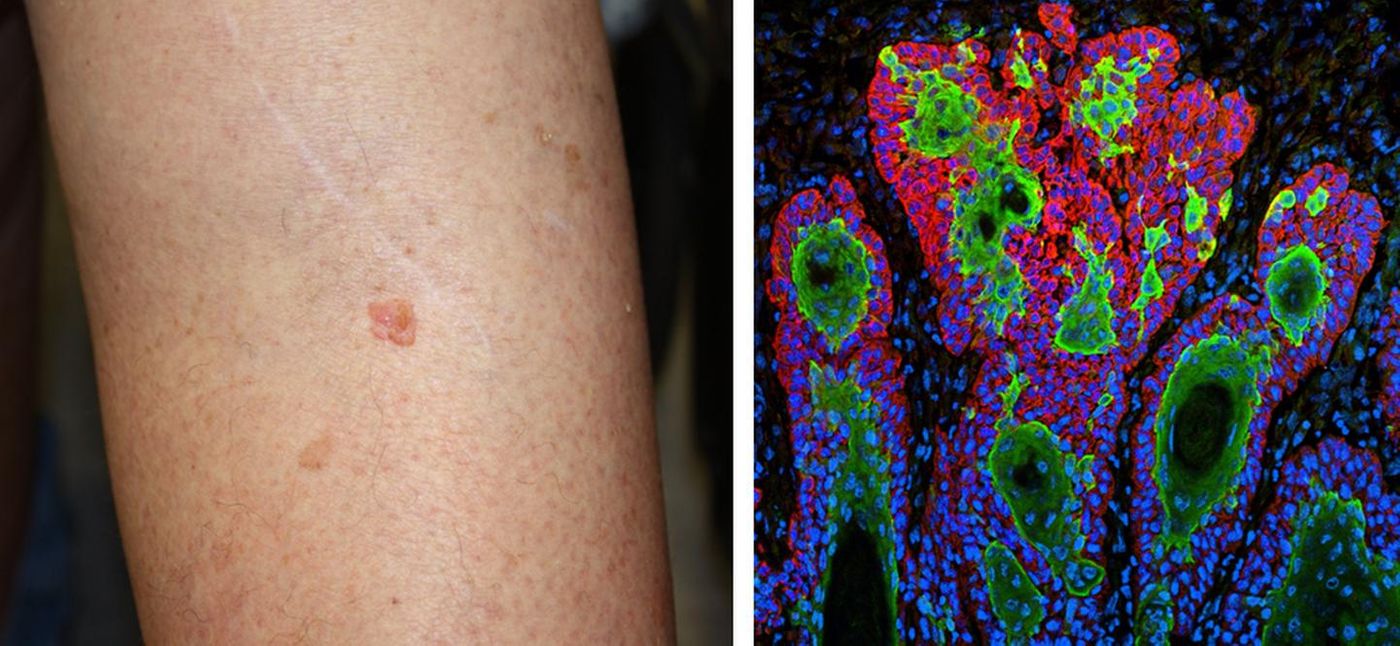
Mohs micrographic surgery (MMS) was developed by Frederic Mohs in the 1930s. It allows a surgeon to methodically remove cancerous tissue in stages during an outpatient procedure. Starting on the surface, a doctor removes cancerous skin growths one layer at a time, examining each one under a microscope, until they reach a point when no abnormal cells are evident. It is intended to remove the tumor to the “roots;” to extensions of the cancer that can run under the skin or along nerves, blood vessels or cartilage. Ideally, it extracts the cancer in meticulous stages without the patient losing a large amount of surrounding healthy skin, especially in areas where it is especially preferable to save the skin, such as on the nose. The Mayo Clinic explains this technique “is for larger, recurring or difficult-to-treat skin cancers, which may include both basal and squamous cell carcinomas.”
Should the Stages of Mohs Surgery Be Reduced?
In 2019, researchers from Johns Hopkins Medicine and seven partnering health care organizations released a study on the use of MMS that determined some surgeons might be excising “more-than-necessary” amounts of tissue.
“Wide surgeon-level variation exists in the mean number of staged resections used to treat a tumor, resulting in a cost disparity and question of appropriateness,” the study states.
The conclusion that some surgeons were carrying out too many stages of tissue removal was based on a 2014 study they carried out of 2,329 U.S. surgeons who each performed more than 10 MMS procedures that year. They used an American College of Mohs Surgery (ACMS) measurement system, in which a surgeon's annual mean stages per MMS case determines the “measure of quality and appropriateness for the technique.” This metric allows ACMS to identify physicians deviating from the average as “outliers” who perform excessive stages in MMS. The research team relied on this system to identify outliers and then studied whether a related “Dear Colleague" performance evaluation letter sent out in 2017 could alter these surgeons’ behaviors -- it did.
The researchers divided the study population into four groups: outliers who would receive an intervention letter indicating their performance and urging “an improvement in practice,” outliers who would not receive an intervention letter, inliers who would receive a performance evaluation, and inliers who would not receive a letter.
The study reports that the notified outlier group responded with a pre- to post-intervention decrease in mean stages of surgery per cancer case, with 83 percent changing their MMS behavior. The non-notified outliers also dropped in mean stages carried out, with 69 percent altering their MMS choices. The change in behavior among non-notified outliers was attributed to an awareness campaign “and possible communications between surgeons who received the letters and their colleagues who did not.”
"This study demonstrates the tremendous power of physicians within a specialty to create peer-to-peer accountability and of using that accountability to reduce unnecessary treatment and lower health care costs," Martin A. Makary, M.D., Ph.D., said. He is the senior author of the study, a professor of surgery at Johns Hopkins and the principal investigator at Improving Wisely, an organization that seeks to lower medical costs “by implementing measures of appropriateness in health care.”
Sources: The Mayo Clinic, EurekAlert, JAMA Dermatology