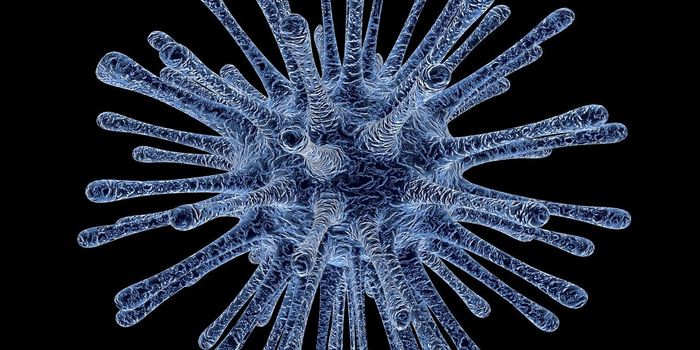
The culprits in a rare immune cell cancer called cutaneous T-cell lymphoma may be a group of mutations in 15 genes for proteins that work together in a T-cell-survival mechanism. When the mutations keep the mechanism from turning off, the T cells keep multiplying. Researchers at the
Stanford University School of Medicine have identified the mutations, which may help to determine treatments for a condition that is currently incurable. The findings were published online August 10 in Nature Genetics and reported in
Drug Discovery & Development.

Rashes, skin tumors and leukemia are manifestations of cutaneous T-cell lymphoma, which responds poorly to traditional chemotherapy. A technique called total skin electron radiation that was developed at Stanford has some effect on it. A new stem cell transplant therapy, also developed at Stanford, has potential for long-term remission for people with advanced, high-risk cutaneous T-cell lymphoma.
Because the role of the proteins has been identified, new strategies can be developed for fighting the disease. Now researchers can seek drugs to diminish the malfunctioning proteins from the mutations.
According to Youn Kim, MD, professor of dermatology and one of the paper’s authors, “We can now design drug trials in a smart, evidence-based way that is specific to the patient.”
Before doctors can prescribe drugs targeted to specific proteins, they have to determine which mutations in the cell-survival pathway their patients’ malignant T cells carry. Such mutations were not present in 60 percent of these cancers sequenced by the researchers.
As senior author Paul Khavari, MD, PhD, professor and chair of dermatology, explained, “It really highlights that the future of many types of cancer treatment is going to be: first, know the cancer by sequencing it, and then tailor the therapy specifically.”
Four of the patients had a mutation that replaced a specific amino acid in the tumor necrosis factor receptor 2, a protein in the cell membrane that gets signals from outside the cell. Because of the mutation, the receptor was locked into an always-on state, keeping the cell-survival pathway from shutting down. Previous studies showed that patients who had increased TNFR2 protein in their bloodstream had more aggressive forms of the cancer that were more likely to recur after treatment. Thus, the researchers looked at the other patients’ DNA to determine whether duplications triggered the elevated levels in the blood and heightened signaling to activate the cell-survival pathway. They determined that 10 of the patients had multiple copies of the TNFR2 gene and then confirmed the biological role of TNFR2 by growing cells in the lab with either the amino acid mutation or the duplicate TNFR2 genes and demonstrating that the cell-survival pathway was more active than normal cells.