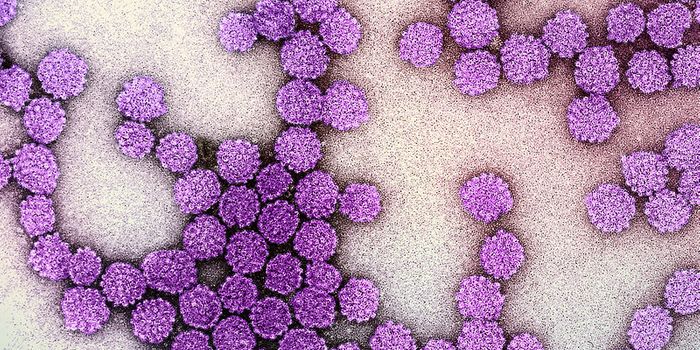
Active surveillance could be a viable alternative to surgery and radiation for some women with ductal carcinoma in situ, or DCIS, according to a new mathematical model.
The watch-and-wait approach is a particularly good option for older women and women with other serious health problems, researchers say, adding that accurate staging at the time of diagnosis would markedly improve any approach.
“We currently lack the ability to determine whether the clusters of cells diagnosed as DCIS will remain harmless or progress,” says senior author E. Shelley Hwang, chief of breast surgery at the Duke University Cancer Institute. “As a result, we treat them all upon diagnosis as if they are invasive cancer, using a combination of surgery, radiation, and hormonal therapy.
“There is growing concern that we may be causing harm by using aggressive procedures for some conditions that may never cause illness or death,” Hwang says. “Our study was designed to provide some guidance for an alternative approach.”
More than 50,000 women a year in the United States are diagnosed with DCIS, which is considered the earliest form of breast cancer, and most women who are diagnosed—97 percent—undergo aggressive treatment. It is unknown how many of those diagnoses would have progressed to invasive cancer had they not been treated, but estimates range from 20 percent to 50 percent.
The biggest hurdle to understanding that risk is a lack of clinical trials in which women diagnosed with DCIS are randomly assigned to either receive current treatment or active surveillance.
To fill that void, at least partially, researchers set about building a mathematical model to determine when active surveillance might be a viable alternative, using data from the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute.
The team, including mathematicians and biostatisticians, created a risk projection model for mortality from all causes among women in different age groups, presenting their results for ages 39-41, 54-56, and 69-71.
They then used the projection model to evaluate how active surveillance would compare to usual treatment as a risk for death, relying on current estimates of disease progression, screening accuracy, and other variables.
Risk over usual care
The findings, published in the
Journal of the National Cancer Institute, show that active surveillance for DCIS added no heightened risk of death for women ages 69-71 compared to current cancer treatment of DCIS, and it was nearly six times less lethal than other competing health conditions in this age group. As a result, active surveillance could be especially beneficial to older women who have serious health conditions such as heart disease.
For younger women—those between the ages of 39 to 41—active surveillance did pose a substantial risk over usual care.
Women in the 54-56 age group were found to have a small elevated risk of breast cancer death with an active surveillance approach compared to usual care, but active surveillance posed no greater risk than other potential causes of death.
The findings could be used to help design a clinical trial in which active surveillance is tested against the usual treatment.
“In the absence of clinical trial data, the best we can do is aggregate relevant available evidence to develop mathematical models to calculate best-possible estimates for the outcomes of active surveillance,” says visiting scholar and lead author Marc Ryser. “Our model suggests that active surveillance may be a rational trade-off for carefully selected patients with DCIS. We hope that this model will help provide additional support for a clinical trial to test whether this is true for some patients.”
The projection models depend on screening frequency, diagnostic accuracy, and screening sensitivity, Hwang says.
“The ability to rule out concurrent invasive cancer at diagnosis is most critical for reducing mortality. We need more accurate biopsy techniques and improved imaging modalities, and these will increase the effectiveness of all treatment approaches.”
The National Institutes of Health, the Swiss National Science Foundation, the National Cancer Institute Early Detection Research Network, and the NIH Provocative Questions Initiative funded the work.
Source:
Duke University
This article was originally published on
futurity.org.