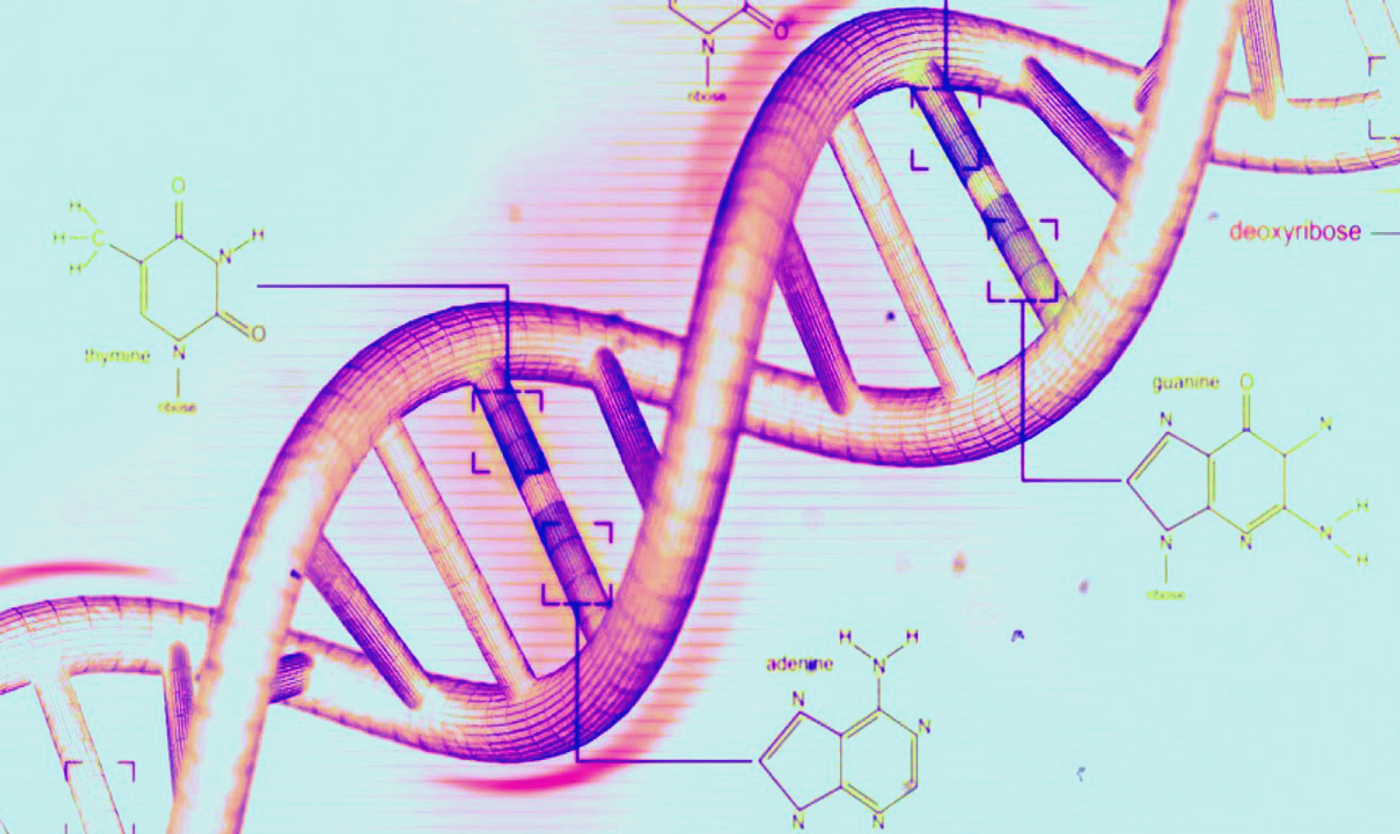
FDA Approves Genomic Profiling Tests to Improve Cancer Care
In December 2017, the Food and Drug Administration (FDA) approved a new genomic profiling test – the second in two months. This test, known as FoundationOne CDx (F1CDx) identifies alterations in a patient’s genes and can be used as a companion diagnostic screen for 15 therapies treating five cancers: non-small cell lung cancer, melanoma, breast cancer, colorectal cancer and ovarian cancer.
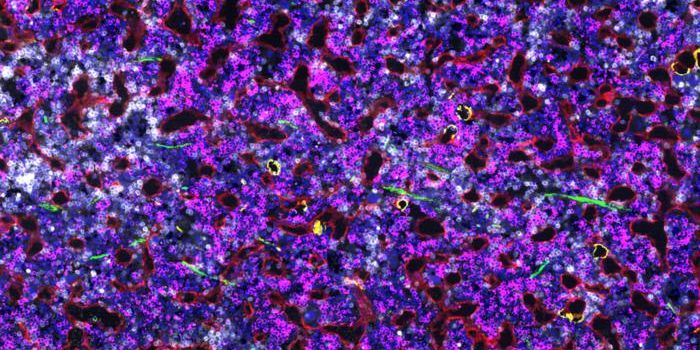
When used as a companion diagnostic, F1CDx determines if a certain therapy is viable for a patient based on whether their tumor displays a specific genetic alteration. It can identify alterations associated with cancer in 324 genes and two kinds of genomic signatures in solid tumors. F1CDx can detect specific mutations accurately 95 percent of the time.
"It's essentially individualized, precision medicine," Director and Chief Medical Officer for the Centers for Medicare & Medicaid Services (CMS) Kate Goodrich says of the newly approved test. When the FDA approval of F1CDx was announced in December, CMS also proposed national coverage for the test, along with other screenings offering next-generation gene-sequencing. This proposal is called a national coverage determination and requires a 30-day public comment period before being formalized.
Also, in November 2017, the FDA authorized a genomic profiling test called MSK-IMPACT. This test was developed solely for New York’s Memorial Sloan Kettering Cancer Center (MSKCC). It is able to scan tumor tissue samples for 468 cancer-associated alterations or mutations.
MSK-IMPACT has been shown to be able to identify actionable mutations (those that can be targeted with a known, approved drug or with one in a clinical trial) in 37 percent of patients with advanced solid cancers.
F1CDx and MSK-IMPACT are known as multigene tests and can retrieve a wealth of information from one tissue sample. Dr. Tracy Lively, chief of the Diagnostics Evaluation Branch of The National Cancer Institute (NCI)’s Division of Cancer Treatment and Diagnosis says this is very helpful because it can be hard to get ample tissue from a single biopsy for multiple unique tests.
“Both tests enable physicians to look at a broad range of genetic abnormalities in their patients’ tumors, some of which might be tied to particular approved drugs and some of which might be useful for other reasons,” she adds. One other potential use for the identification of tumor abnormalities she mentions is finding patients who can participate in clinical trials.
The NCI reports that the FDA also presented a streamlined regulatory approval process in 2017, which makes it cheaper and quicker for hospitals to get FDA authorization for in-house tumor-profiling tests. Lab tests that a single hospital develops and uses only in-house currently do not require FDA authorization to be used.
The FDA also approved a sequencing-based test called the Oncomine Dx Target Test in June 2017. This test was designed for patients who have lung cancer by the biotech company Thermo Fisher.