Fixing What Goes Wrong During Sepsis
A lot of things go wrong during sepsis, but one of the worst is heart complications. In the past researchers determined that boosting energy production in the heart could help, but they didn’t know why. The most recent study, from the same group of scientists, provides an explanation and a plan of action.
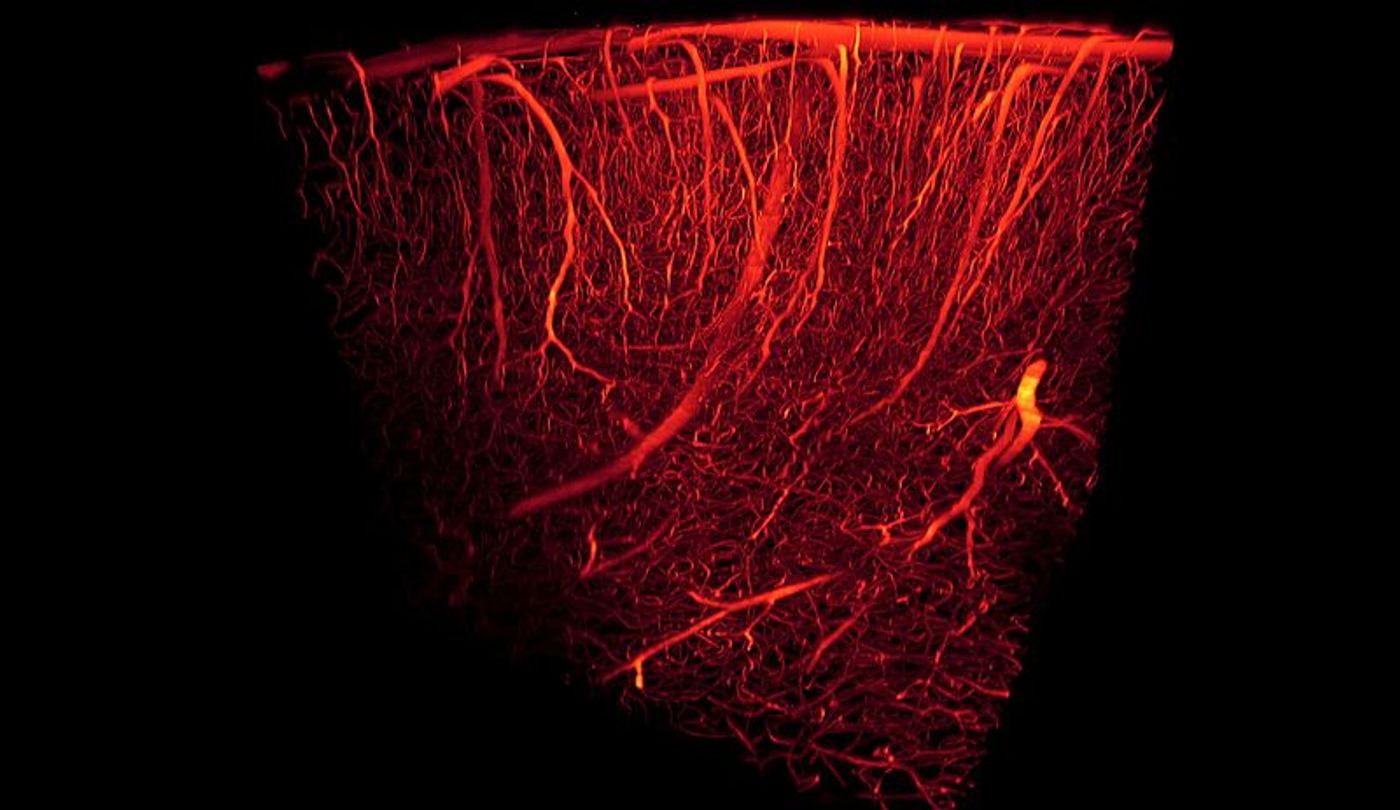
Sepsis is an extreme overreaction to a bacterial infection, causing blood clots, faulty blood vessels, and organ failure. Heart complications are responsible for 80 percent of sepsis-related deaths, and scientists from Temple University want to alleviate some of the devastation with their new findings.
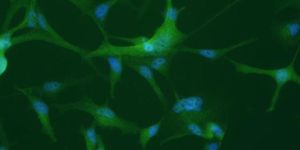
What happens to the heart during sepsis? It becomes weak and fails to generate enough energy to pump effectively due to systemic inflammation. When the heart can’t pump effectively, oxygenated blood doesn’t make it to the cells and tissues of the body, and organ failure ensues. The new Temple University study began to identify and explain the mechanism responsible for the heart’s loss of energy during sepsis. If they can prevent the heart from losing energy, they could potentially increase the amount of time anti-inflammatory drugs have to be effective to treat sepsis.
“Anti-inflammatory therapies fail to improve survival,” explained senior investigator Konstantinos Drosatos, PhD. “We think that this happens because there simply is not enough time for the anti-inflammatory drugs to begin working before critical organs begin to fail."
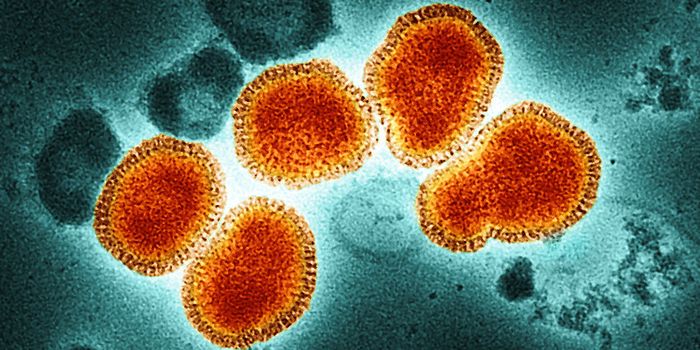
Konstantinos and her team worked with a mouse model of sepsis, treating heart muscle cells with lipopolysaccharide, an endotoxin produced by many types of bacteria that triggers the immune system and induces sepsis. However, they blocked activation of NADPH oxidase 2 (NOX2), an enzyme active during infections that can become toxic if overproduced. They knew to do so because of its connection to boosting oxidative stress in the heart.
"Increased levels of reactive oxygen species are a key feature of cardiac dysfunction during sepsis," Drosatos explained. "Mitochondria, the energy powerhouses of cells, are especially vulnerable to damage from reactive molecules, and this seems to be critical for energy production in the heart and maybe other organs."
Inhibiting the activity of NOX2 lowered oxidative stress in the face of sepsis, and it boosted the heart’s ability to produce energy. Drosatos believes that blocking NOX2 along with applying traditional drugs could increase survival following sepsis and wants to pursue human clinical trials in the near future.
"With our latest findings, supportive and anti-inflammatory treatments would remain a mainstay,” Drosatos explained. “But by also ensuring that the heart is producing energy, we could provide extra time for the treatments to work before the heart fails.”
The present study was published in the Journal of Clinical Investigation Insight.
Sources: MedlinePlus, Journal of Endotoxin Research, Cellular & Molecular Immunology, Temple University Health System