Extracellular Vesicles Help Heart Cells Survive a Heart Attack
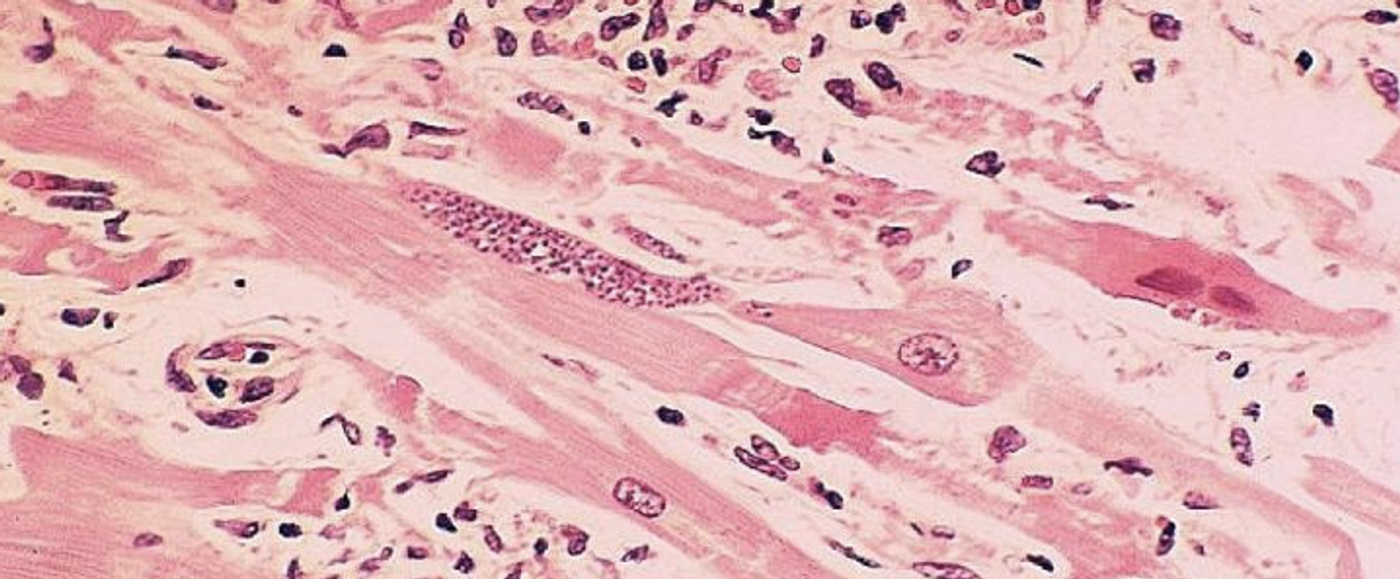
During a heart attack, blood flow is blocked and cells lose oxygen and begin to die. Scientists are developing many new ways to treat heart attacks, some of which involve stem cells, while others utilize different technologies. Extracellular vesicles (EVs) are normally used to ferry biochemical signals or cargo from one cell to another, and they are another promising therapeutic avenue for a variety of disorders. EVs that are isolated from stem cell colonies have already been shown to improve the health of heart cells after a heart attack. Researchers have now learned more about how EVs from vascular cells can be used as a therapeutic.
This research, which has been reported in Science Translational Medicine, has also shown that EVs seem to be able to help cells maintain function even during a heart attack when they are deprived of oxygen. In this work, the researchers used a model of a heart on a chip, which is a tiny device with channels for liquids and cells. The heart-on-a-chip is meant to model heart cell function but is also embedded with sensors that can track the cells as they contract.
"Our organ-on-chip technology has progressed to the point where we can now fight drug targets instead of fighting the chip design," said senior study author Kit Parker, the Tarr Family Professor of Bioengineering and Applied Physics at Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS). "With this study, we have mimicked a human disease on a chip with human cells and developed a novel therapeutic approach to treat it."
While it seems like restoring blood flow to the heart would help during a heart attack, it can actually cause more cell damage, called ischemia-reperfusion injury (IRI) or reoxygenation injury. Cells respond to IRI in multiple ways, and the complexity is a major challenge for treatment development, noted the first author of the study, Moran Yadid, a postdoctoral fellow at SEAS and The Wyss Institute for Biologically Inspired Engineering.
The researchers assessed the proteins in EVs that come from vascular tissue, called endothelial-derived EVs (EEVs). Because they sense hypoxic stress, the researchers thought they may also ferry protective cargo to cardiac cells.
"Surprisingly, even though these vesicles are only a hundred and fifty nanometers in diameter, they contain almost 2,000 different proteins," said Yadid. "A lot of these proteins relate to metabolic processes like respiration, mitochondrial function, signaling, and homeostasis. In other words, a lot of processes that relate to the cardiac response to stress. So, rather than one molecule that is therapeutic, we think that the exosomes contain a cocktail of molecules and proteins that can, all together, help the cell maintain homeostasis, deal with the stress, modify metabolic action and reduce the amount of injury."
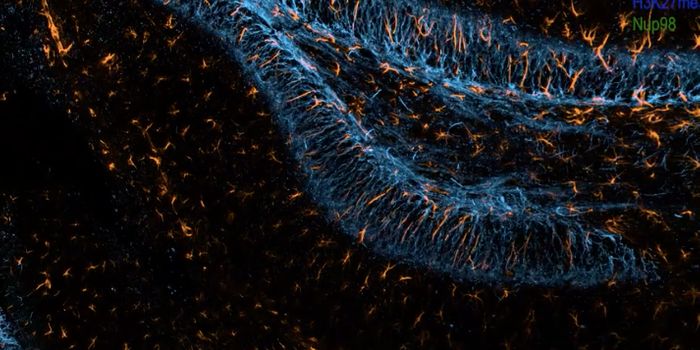
The researchers used the heart-on-a-chip to test the impact of EEVs by simulating a heart attack and deoxygenation, and exposing them to EEVs or not. The cells that were treated with EEVs had better responses to stress and could sustain a higher workload. Chips treated with EEVs had half the cell death and four times the contractile force than untreated ones. After EEV treatment, the pattern of protein expression in injured heart cells was more like that of uninjured cells; these treated cells were also able to keep contracting in the absence of oxygen.
"Exosomal cell therapies might be beneficial when the traditional model of one molecule, one target just won't cure the disease," added Parker. "With the vesicles we administered, we believe we are taking a shotgun approach to hitting a network of drug targets. With our organ on-chip platform, we will be poised to use synthetic exosomes in[a] therapeutic manner that may be more efficient and amenable to more reliable manufacturing."
Sources: Science Daily via Harvard John A. Paulson School of Engineering and Applied Sciences, Science Translational Medicine