A Better Understanding of VLCADD May Improve Treatment
With newborn screenings, clinicians can now identify newly born infants that carry genetic mutations that will lead to disease, sometimes long before those symptoms appear. Some of these genetic diseases cause the loss of an important molecule or enzyme, and in some cases, a newborn screen allows doctors to apply a therapy that prevents the worst consequences of that disease in a patient.
VLCADD (Very long chain acyl-CoA dehydrogenase deficiency) affects about one in 40,000 births. Fatty acids are a crucial source of energy. The genetic mutation disrupts an enzyme that breaks down very long chain fatty acids, so the body cannot generate energy from fat. Symptoms may be brought on by periods of fasting or exercise. The disorder can lead to low blood sugar and heart failure if it's not treated.
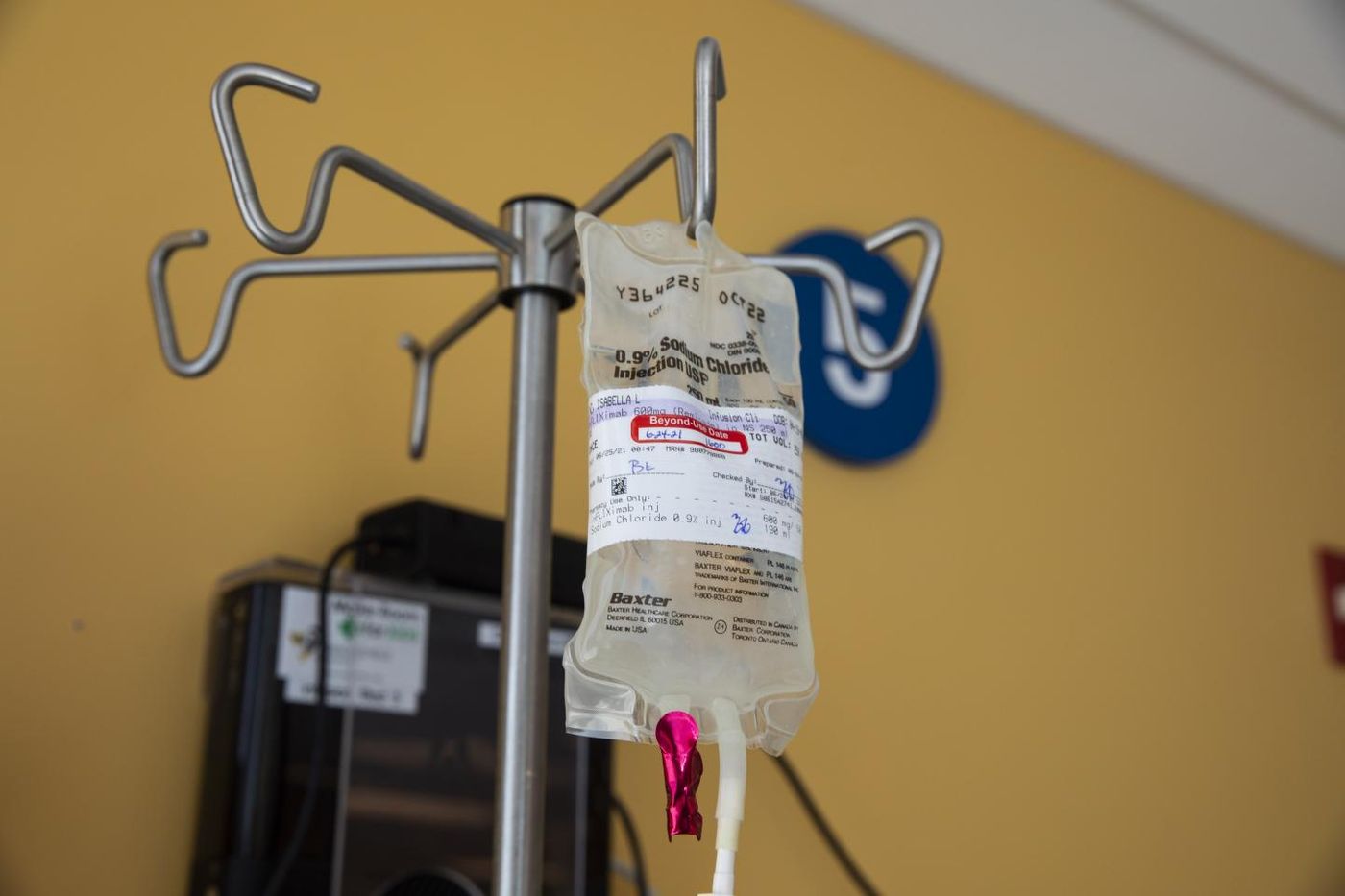
One way to treat the disease is to limit the amount of very long chain fatty acids that patients consume while increasing starch and medium chain triglyceride intake, along with a drug that's recently been approved. This can help manage the disorder.
However, muscles may still break down in these patients, a condition called rhabdomyolysis, which can cause severe pain. Therefore, researchers thought that another biochemical pathway was likely involved.
"These episodes looked a lot like inflammatory muscle disease, but usually that is persistent and doesn't wax and wane, so it wasn't a perfect fit," said senior author Jerry Vockley, M.D., Ph.D., chief of Genetic and Genomic Medicine and director of the Center for Rare Disease Therapy at UPMC Children's Hospital of Pittsburgh. "Still, I couldn't shake the thought that there was some inflammatory link, so we tested patient blood samples. Sure enough, when the episodes were happening, certain inflammatory markers were high, and when the patients were well, they were lower. Knowing this will allow us to try to figure out why this inflammation is happening and prevent it."
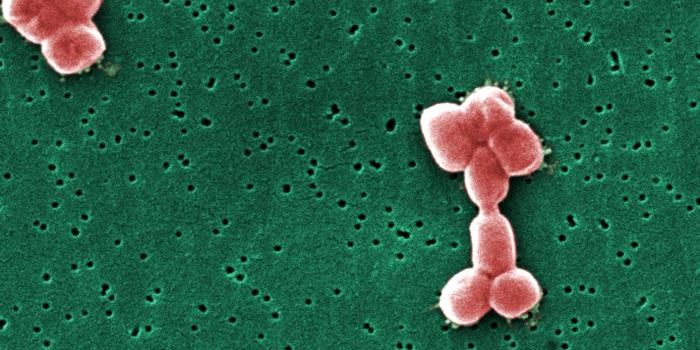
Vockely's team was able to use samples from VLCADD patients, including one patient that volunteered to routinely give blood over several years. The scientists found that during attacks of rhabdomyolysis, there were elevated levels of inflammatory molecules called cytokines; the patients were experiencing what's known in the clinic as a cytokine storm, where immune molecules begin to attack the body's tissues. Even when patients were not having a bout of rhabdomyolysis, their immune marker levels were abnormally high. The findings have been reported in Clinical & Translational Immunology.
However, the researchers still have more to learn about what's underlying this immune dysfunction.
"The cytokines activate cells, but those cells aren't following the rules. In the immune system, cytokines and cells talk to each other to regulate and counter-regulate their actions accordingly. But that's not happening the way you'd expect in VLCADD patients," explained study co-author Abbe de Vallejo, Ph.D., associate professor of pediatrics, immunology and rheumatology in the University of Pittsburgh's School of Medicine. "It's paradoxical and is our next challenge. If we can find the disconnect, we may be able to learn what is triggering the inflammatory response and stop it from happening altogether."
While more work will be needed, the researchers have found some treatment success by giving VLCADD patients anti-inflammatory medications that can relieve and prevent acute rhabdomyolysis.
Sources: AAAS/Eurekalert! via University of Pittsburgh, Clinical & Translational Immunology