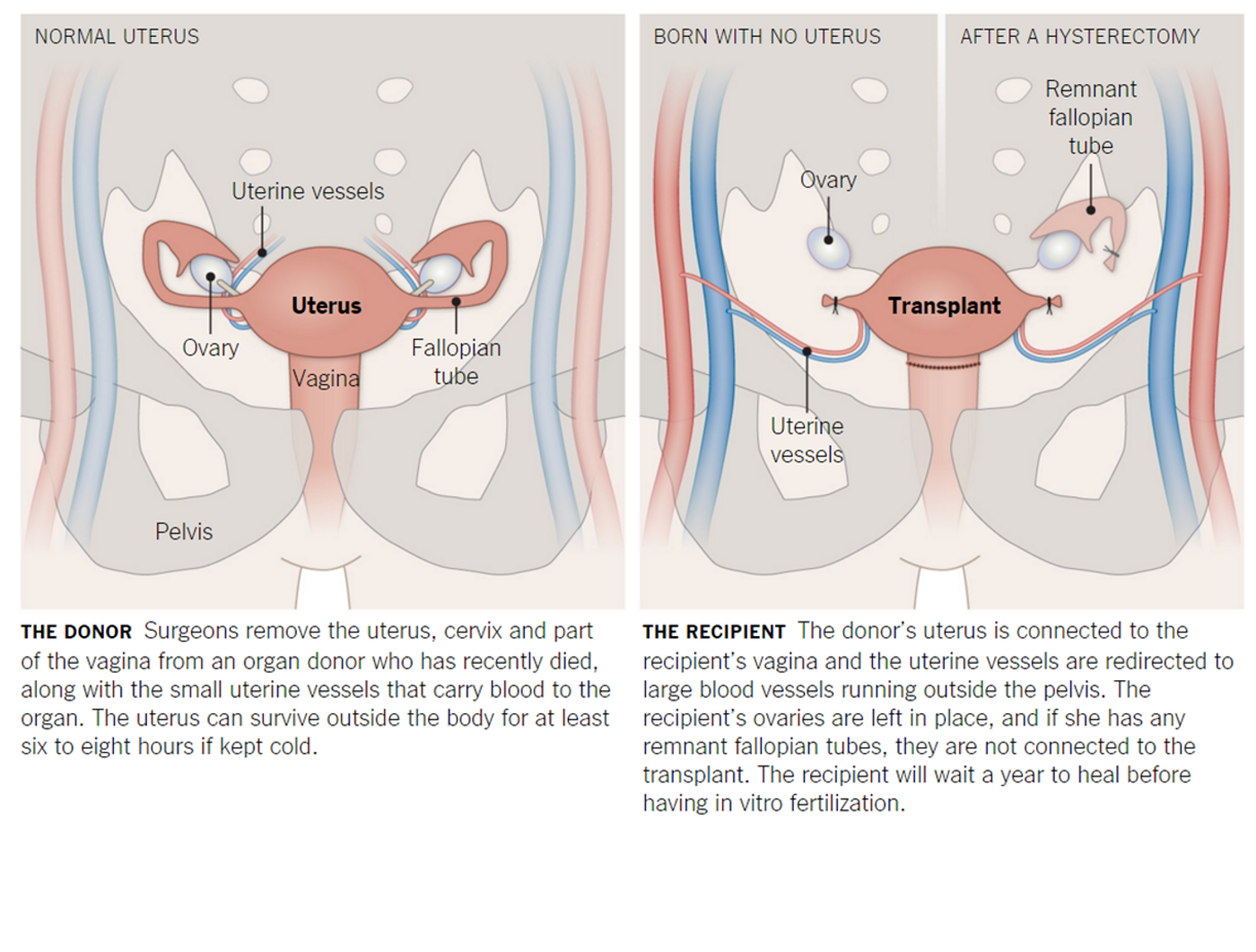
As organ donors, people consent to donating their vital organs after death, such as the heart, lungs, liver, and kidneys, to save another person’s life. For female donors, the organ list may soon include the uterus. Following the steps of the successful uterine transplants in Sweden, U.S. doctors at the
Cleveland Clinic are setting up a trial to give 10 women a chance to be pregnant.
The clinical trial is specifically for healthy women who suffer from uterine factor infertility (UFI). This condition prevents pregnancy because the uterus is missing or non-functional, either because of congenital defects or trauma sustained extrinsically. While there are options for women to become mothers, “There are women who won’t adopt or have surrogates, for reasons that are personal, cultural or religious,” said Dr.
Andreas G. Tzakis, lead investigator of the trial. Furthermore, the uterine transplant is the only option that would allow a woman with UFI to biologically carry her own baby.
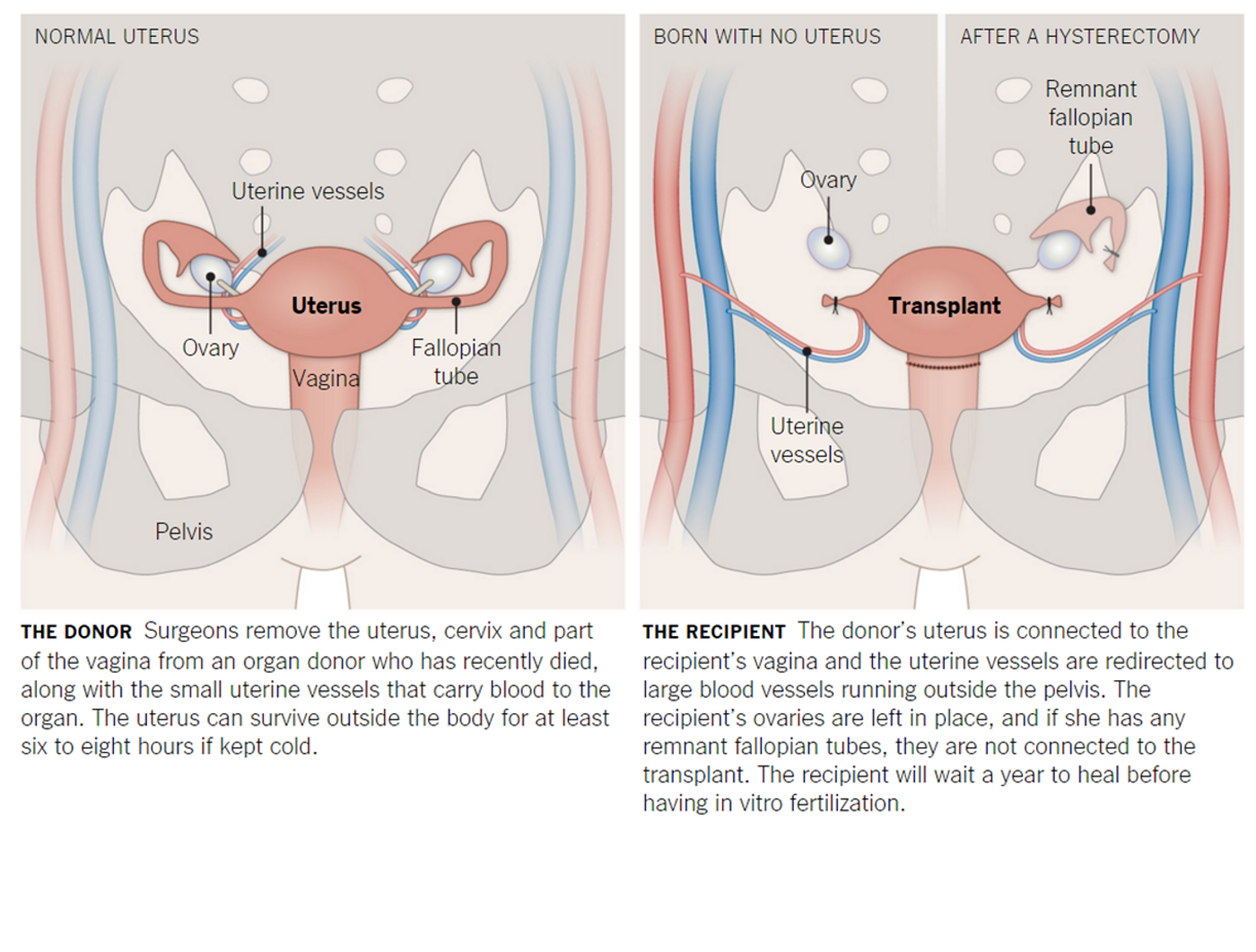
The procedure requires extensive planning with many steps lined up even before the transplant happens. To select the prospective recipient of a uterus, the team meticulously screened applicants for eligibility, factoring in mental and physical health, relationship status, and financial stability. Once selected, the women will undergo ovarian stimulation treatment to allow 10 eggs to be collected. Doctors will then use in vitro fertilization (IVF) to fertilize her eggs with her partner’s sperm. The 10 fertilized eggs will wait, frozen, for a year or more before implantation.
Once a compatible uterus is harvested from a deceased donor, doctors will transplant the donated organ into the recipient. The actual transplant process takes a mere six to eight hours; however, it takes a whole year for the donated uterus to completely heal inside the recipient’s body. After this period, the frozen fertilized eggs are thawed and implanted, one at a time, into the recipient’s uterus until she becomes pregnant. Throughout pregnancy up to delivery, the mother-to-be is monitored closely by a high-risk obstetrics team. In addition to taking immunosuppressant drugs to prevent organ rejection, she will also undergo monthly cervical biopsies to confirm the organ is still intact. The birth of the baby is strategically carried out via a scheduled cesarean section to prevent labor strains to the transplanted uterus.
Preserving the transplanted uterus is critical for women who elect to be pregnant again, as doctors will implant another of the in vitro fertilized eggs that she has in reserve. But because pregnancy requires the woman to be on anti-rejection medications, the team has put a limit of two babies for the transplanted uterus. Once the pregnancy is over and the medications stopped, and the transplanted uterus can either be surgically removed (hysterectomy) or allowed to wither away inside the body.
So far the
University of Gothenburg in Sweden has the claim on the only successful births resulting from uterine transplants. Of nine women who underwent the procedure, four gave births to
healthy but premature babies, while two transplants failed and necessitated removal. Another woman from that cohort is due in January.
While the uterine transplant is considered a “life-enhancing” procedure, it carries the same level of risks as for any lifesaving organ transplantation. The biggest risk of all is organ rejection, which means that “this dream does not always have a happy ending,” cautions Dr. Tristi Muir, chair of the Department of Obstetrics and Gynecology at Houston Methodist Hospital.
“Less than 50 percent of the women who have undergone uterine transplantation have had a baby,” she says. “There are risks to the woman undergoing a transplant including surgical risks and medical risks of rejection and suppression of the immune system to tolerate the transplant. [And] the financial impact on a family and our healthcare system of the cost of transplantation, immunosuppression, and prematurity should not be lost in chasing this dream.” – Dr. Tristi Muir
To minimize complications, only healthy women who meet the team’s stringent criteria will be eligible. In addition, Dr. Tzakis and his team will transplant uterus obtained from deceased donors, removing donor-related complications. And because the transplanted uterus will be removed eventually, its effects are temporary.
“Unlike any other transplants, [uterine transplants] are ephemeral. They are not intended to last for the duration of the recipient’s life, but will be maintained for only as long as is necessary to produce one or two children.” – Dr. Tzakis
Already eight women from across the country are already hopeful to be recipient of uterine transplants. For these women and countless more, this clinical trial will provide hope for an experience that they could never have on their own.
Sources:
Cleveland Clinic,
Yahoo,
The NY Times,