Certain Air Pollutants Linked to Worse Outcomes in Interstitial Lung Disease
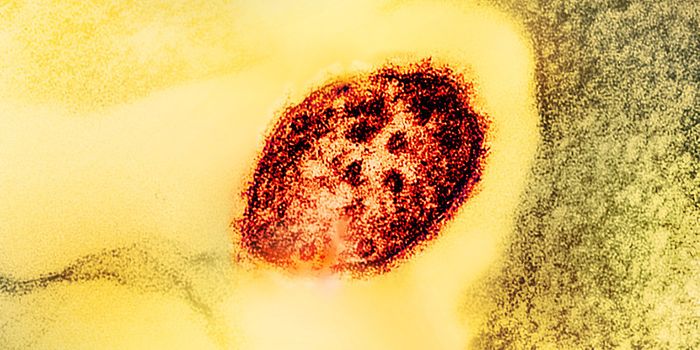
Fibrotic interstitial lung disease (fILD) is a frustratingly difficult disease to characterize. For one, fiLD is difficult to diagnose at the time that symptoms begin to occur. In laboratory imaging, fiLD presents as lung fibrosis, a symptom that is shared by multiple lung disorders.
Clinicians are typically unable to diagnose a patient with fiLD until a high-resolution computed tomography (HRCT) study has been completed. Patients with fILD typically experience a diminished ability to breathe as a result of progressive scarring of the lung tissue.
Gillian Goobie, M.D. and doctoral candidate in the Pitt School of Public Health, says that “some people with these lung diseases have an expected lifespan from diagnosis to death of only a few years, and yet it’s a mystery as to why they developed the disease, why their lungs become so scarred.”
Though the cause or causes of fiLD are not yet known, a new study published by JAMA Internal Medicine shows that specific types of air pollution significantly worsen outcomes in individuals with fiLD. This study investigated data from over 6,500 patients diagnosed with fiLD in the United States and Canada.
The researchers also looked at the geographical location of these patients to determine the amount of air pollution they are exposed to. Specifically, the researchers looked at the patients’ exposure to PM2.5, or particulate matter smaller than 2.5 microns. Pollutants of this size are small enough to enter the bloodstream and lung tissue.
The researchers found that fiLD patients living in areas with PM2.5 had progressively worse outcomes as levels of PM2.5 increased. Increasing levels of PM2.5 were linked to more severe disease at the time of diagnosis, quicker disease progression, and death. The researchers found that PM2.5 pollutants specifically from factories, fossil fuel combustion, and agriculture were associated with worse outcomes when compared to PM2.5 pollutants from naturally occurring particulates such as sea salt or soil dust.
Co-author S. Mehdi Nouraie, M.D., Ph.D., says that “ultimately, we want to encourage a data-driven awareness,” Nouraie said. “We want people to think about the quality of the air we breathe. Patients, health care providers and policymakers can all use the new information we’re providing to try to improve health outcomes. When you make the air safe for the most vulnerable to breathe, you’re making it safe for all of us.”
Sources: American Journal of Respiratory and Critical Care Medicine, JAMA Internal Medicine