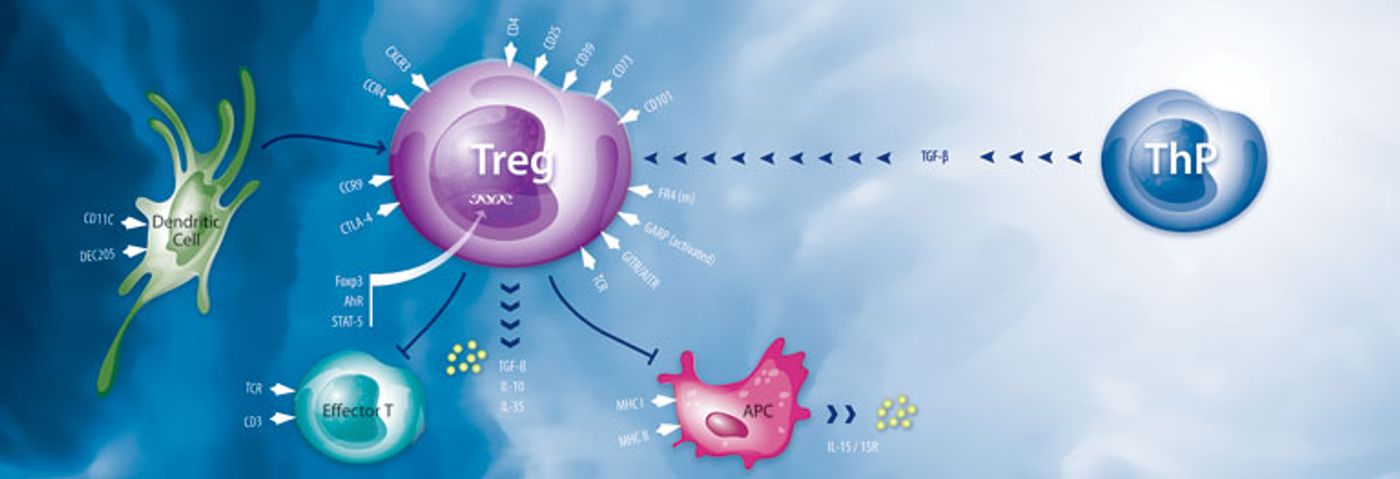
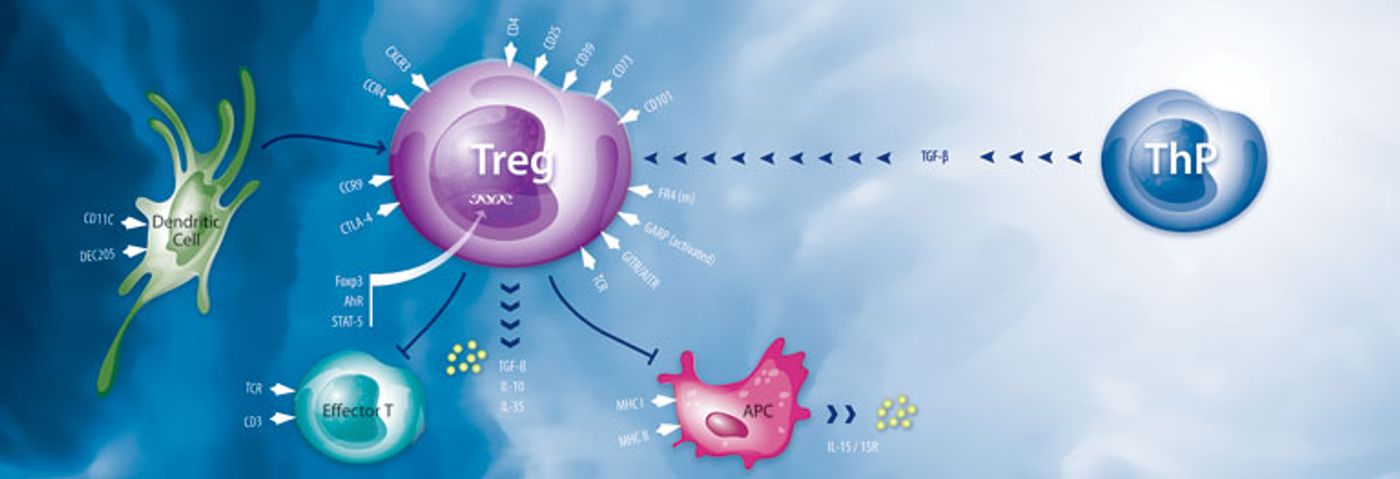
The immune system not only responds to infections and other potentially problematic abnormalities in the body. It also contains a built-in brake in the form of regulatory T cells, or Tregs, that keep inflammatory responses from doing damage. In autoimmune diseases, sometimes these Treg cells act strangely.
A new study led by Songtao Shi, professor and chair of the Department of Anatomy and Cell Biology the School of Dental Medicine of the University of Pennsylvania, has shown how Tregs can be regulated, by hydrogen sulfide, a gas produced by the body’s muscle cells and often associated with the smell of rotten eggs, according to a
press release. The finding, published in the journal
Immunity, suggests several new possible points for therapeutic intervention, with implications for autoimmune diseases as well as other conditions such as cancer and hypertension.
Scientists thought that signaling pathways involve a ligand binding to a receptor, but gases can also trigger signaling cascades in the body. The best known is nitric oxide, or NO, which regulates a host of functions, such as blood pressure. Carbon monoxide is another so-called “gasotransmitter.”
Researchers also understand that hydrogen sulfide gas plays some significant roles in the body. Reduced levels of H2S have been associated with immune disorders, cancer and hypertension.
According to Shi, “H2S is very interesting. High levels of it are toxic, but our body maintains it at a certain level, and our cells produce it.”
Earlier, Shi and colleagues discovered that mesenchymal stem cells produce and rely on H2S for proper functioning. They saw that mice with reduced levels of H2S had problems symptomatic of autoimmune disease.
To discover the exact role of the gas in immune regulation, the research team examined Tregs in culture and determined that they produce H2S. Mice bred to produce reduced levels of H2S had abnormally low numbers of Tregs and developed autoimmune disease that affected multiple organs. Giving these mice compounds that release H2S partially reduced these effects.
Next, the team wanted to find out more about the mechanism of H2S action on the immune system. They had already observed that H2S-deficient T cells had lower levels of a Treg marker called Foxp3, but H2S did not seem to affect the actors of a known pathway by which Foxp3 is produced. They hypothesized that H2S might act in another pathway to regulate Foxp3 expression.
Through a series of experiments, they saw that mice with reduced H2S production had large numbers of methyl groups on the Foxp3 gene, tags that repress the gene’s expression. It was already known that demethylation of Foxp3 can occur through two enzymes called Tet1 and Tet2, which Shi called “a hot area of research right now.”
Their work revealed that H2S regulates the expression of Tet1 and Tet2 by modifying a transcription factor called NFYB by adding a sulfur atom to it, a process called sulfhydration. Reducing H2S levels led to reduced expression of Tet1 and Tet2 in T cells and, consequently, impaired function and development of Tregs. The researchers could partially reverse these effects by adding back a source of H2S.
Shi explained, “This is the first time anyone has connected sulfhydration with Tet and Tet with Foxp3. It’s becoming clear that H2S has a very important role to play in immune regulation.”
Shi and his team are continuing to examine how H2S operates in the context of both stem cells and T cells and are looking to determine whether it plays critical roles in other cell types. They are also following up on the current work to identify ways to intervene when H2S levels fall in order to prevent autoimmune problems.
“There are a lot of different ways to rescue this problem,” Shi concluded.