Scientists have long suspected that respiratory viruses - the sort that cause common colds or bronchitis - play a critical role in the long-term development of chronic lung diseases such as asthma and chronic obstructive pulmonary disease (COPD).
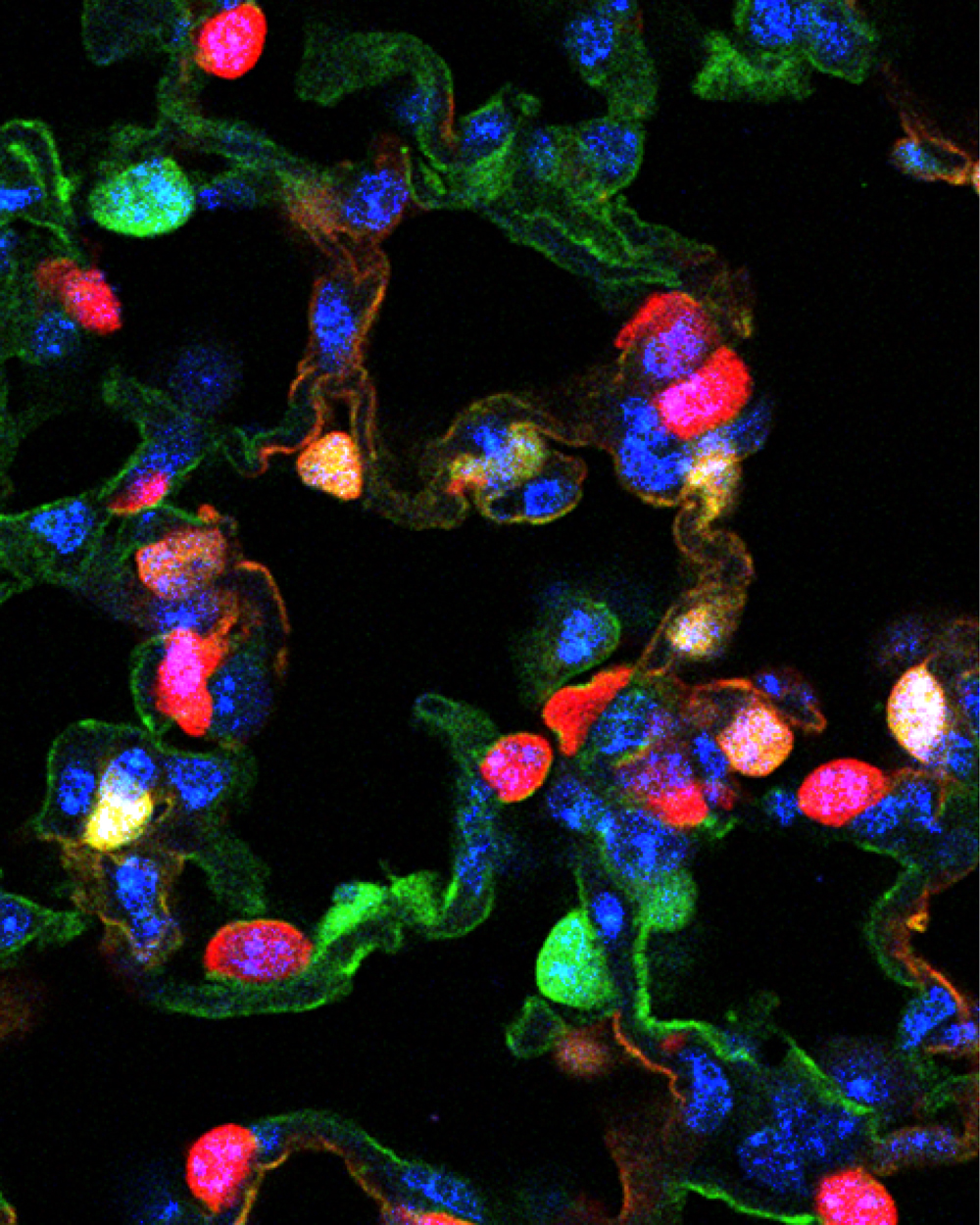
Studying mouse and cell models of this process, researchers at Washington University School of Medicine in St. Louis now have shown how immune cells dispatched to the lung to destroy a respiratory virus can fail to disperse after their job is finished, setting off a chain of inflammatory events that leads to long-term lung problems.
Understanding such details may help scientists find ways to block the accumulation of inflammatory immune cells and prevent progression to chronic lung disorders.
The study appears April 20 in The Journal of Experimental Medicine.
The findings stem from research into immune cells called macrophages.
"In general, scientists thought this type of macrophage was involved in the repair of the lung," said senior author Michael J. Holtzman, MD, the Selma and Herman Seldin Professor of Medicine at the School of Medicine. "That may be true in some cases. But like many things in nature, too much of a good thing can become a bad thing."
When large numbers of this type of macrophage accumulate, they appear to stop orchestrating the immune response against acute viral infections and instead participate in a type of response that is more typically directed against parasites and allergens. Holtzman and his colleagues observed that macrophages producing this type of immune response also express a protein called TREM-2 at high levels.
The new work shows that the usual cell-surface form of TREM-2 is indeed needed to sustain the macrophages as they fight off viral infection and the early illness it causes. Then, after the initial infection is cleared, TREM-2 is cleaved from the outer surface of the macrophages. Previously, this cleaved form of the protein was thought to be inactive.
"We were surprised to find that this cleaved form of TREM-2 is actually quite active," Holtzman said. "It potently prevents the programmed death of macrophages, promoting their survival. So this form of TREM-2 allows for macrophages to hang around longer than they should."
Holtzman noted that TREM-2 enables a feed-forward process for inflammatory disease. Each new infection activates macrophages, which later produce the cleaved form of TREM-2. This form then promotes further macrophage accumulation and ultimately contributes to ongoing and progressive inflammatory disease.
Implicating TREM-2 in the harmful accumulation of inflammatory immune cells opens the door to exploring ways to block it, according to first author Kangyun Wu, PhD, a staff scientist.
"We don't yet have a specific drug to interrupt the TREM-2 process," Holtzman said. "But we now understand the controls for the process, so our drug discovery program is already screening for compounds that might keep TREM-2 at normal levels."
The researchers also found that the cleaved form of TREM-2 that causes the macrophages to stick around when they shouldn't does not appear to be involved in the initial immune response to the acute viral infection. So presumably, blocking it should not interfere with the important task of clearing the respiratory virus from the lungs.
Holtzman also pointed out that individual genetic variation in TREM-2 may explain why some people never develop chronic lung disease even after many viral lung infections.
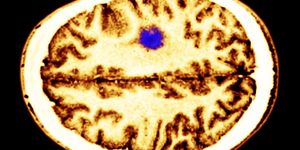
While this study focused on the lung, Holtzman said TREM-2 could be involved in other inflammatory diseases in which the immune system is chronically activated in other organs. He pointed to a possible role in the brain, for example, since related work has associated certain genetic variants of TREM-2 and macrophage dysfunction with Alzheimer's disease.
Source: Washington University in St. Louis


![Master Lab Weighing: Accuracy, Compliance & Audits [eBook]](https://d3bkbkx82g74b8.cloudfront.net/eyJidWNrZXQiOiJsYWJyb290cy1pbWFnZXMiLCJrZXkiOiJjb250ZW50X2FydGljbGVfcHJvZmlsZV9pbWFnZV85MWRmZmRjMDIwNDBlMWJjMzYwN2ZiYWY2ZjI4ZGMzYzBmZGMwZGMyXzkxOTcucG5nIiwiZWRpdHMiOnsidG9Gb3JtYXQiOiJqcGciLCJyZXNpemUiOnsid2lkdGgiOjcwMCwiaGVpZ2h0IjozNTAsImZpdCI6ImNvdmVyIiwicG9zaXRpb24iOiJjZW50ZXIiLCJiYWNrZ3JvdW5kIjoiI2ZmZiJ9LCJmbGF0dGVuIjp7ImJhY2tncm91bmQiOiIjZmZmIn19fQ==)