The Role of the Gut-Lung Axis in the Development of Tuberculosis
A large proportion of current literature is on the gut microbiome, which has been proven an essential part of the immune system and homeostasis within the body. The gut microbiome has been divided into two major phyla--Firmicutes and Bacteroidetes--, but it should be noted that there have been at least 10 different phyla that may have significant contributions to the microbiome. Three predominant genera have been identified--(1) Bacteroides, (2) Prevotella, and (3) Ruminococcus. Lung tissue was previously thought to be sterile and devoid of microorganisms, but research has shown that there is microbiota from the Firmicutes, Bacteroidetes, and Proteobacteria phyla similar to those in the gut.
Recent studies have identified a gut-lung axis, which was initially proposed in the early 1990s based on a hypothesis that bacteria and bacterial endotoxins passed into the bloodstream leading to the release of cytokines, such as TNF-α and IL-6, causing adult respiratory distress syndrome and multiorgan failure. Since its initial conception, the existence of a gut-lung axis has been well-documented and linked to lung disease and changes in immune responses when the bacterial communities are altered.
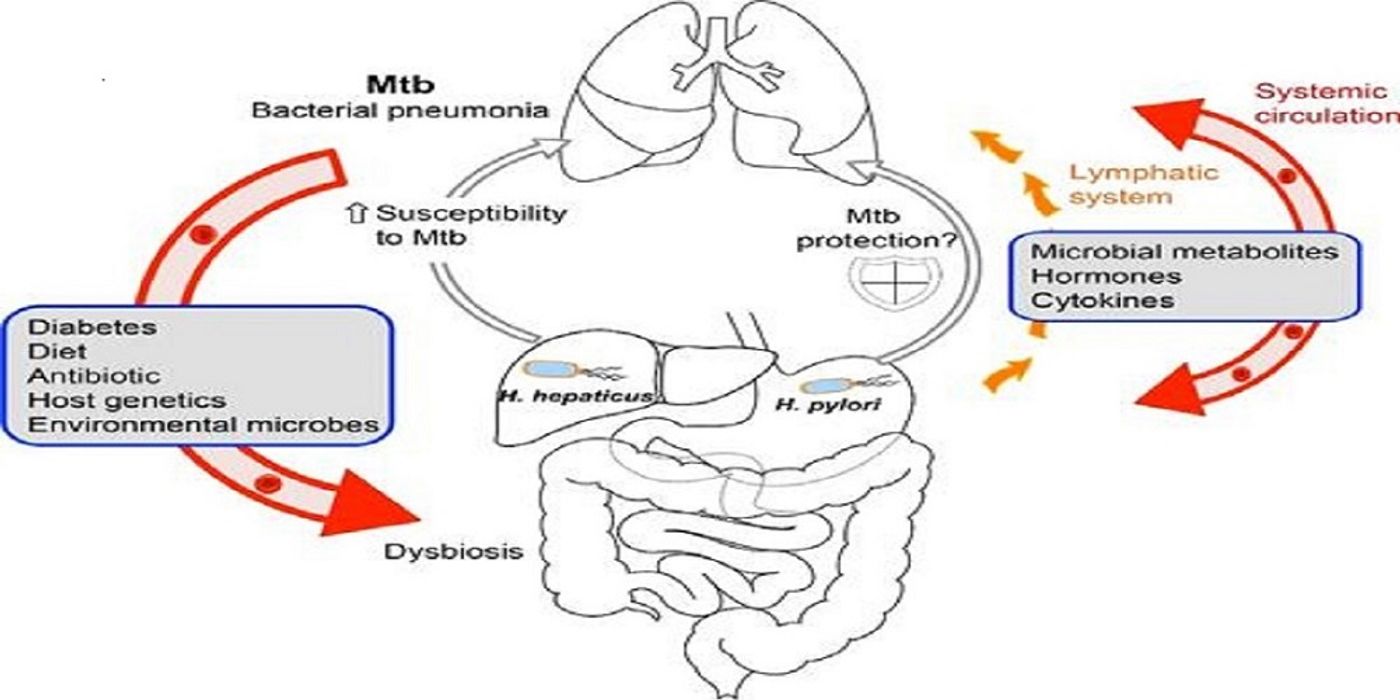
Cervantes and Hong discuss the possible interactions between the commensal bacteria, Helicobacter hepaticus, and pathogenic strains of Helicobacter pylori with the organism, Mycobacteria tuberculosis (MTB). They cite two independent studies that have shown that natural colonization of the GI tract causes changes in the microbiota and leads to susceptibility of the immune system to MTB and injury to lung tissue. In comparison, H. pylori, which is found in about half the human population, appears to be an immune modulator resulting in reduced inflammation commonly seen in inflammatory bowel disease and Salmonella infections.
Figure 1. Gut-Lung Axis in MTB Infection. Credit: Cervantes and Hong
Figure 1 depicts the passage of products into the bloodstream making the connection of the gut-lung axis. It also shows how metabolic diseases and other conditions can affect susceptibility to MTB. The gut-lung axis is bidirectional, and a lung-gut axis exists where inflammation in the lungs can change the microbiota found in the gut. Recent studies have found that pneumonia caused by Pneumocystis jirovecii and infection with MTB both produce changes in the gut. It is also hypothesized that the liver and the lymphatic system may be involved when immune cell activation by macrophages and neutrophils occurs.
The authors conclude that the use of prebiotics and probiotics may be a potential mediator for respiratory diseases, and there have been promising results that introduction of Lactobacillus into the gut may prevent Pseudomonas lung infections. The possible protective features of the intestinal system on lung health may be developed into an adjunctive therapy against MTB.