New Male Contraception Boasts 2.5 Hours of Infertility
No other healthy cell in the human body has a bigger target on its head than sperm. Scientists have tried to eradicate its development with hormones, targeted its proteins, and tried to chop off its tail.
We’ve been promised the “male pill” and the “male IUD” for decades. Breakthrough studies are released with fanfare only to yield lackluster clinical trial results. Today, the Levin pharmacology laboratory of Weill Cornell Medicine is announcing an exciting new approach to male contraception in Nature Communications. But will it break our hearts like all the others?
The number of contraceptives available to sperm-producing humans is a paltry two. The vasectomy was popularized during World War II and is considered non-reversible. The last flexible form of male birth control was released for mass production 150 years ago. The condom has a 95% effectiveness, much to the shock and chagrin of sexually active and non-reproducing adults.
Condoms and vasectomies just aren’t cutting it (no pun intended). The UN predicts that the earth’s population will grow from 8 billion to 10.4 billion by 2100, presenting a challenge for sustainable growth. Half of all pregnancies are unplanned, leaving women, families, society, and the environment to pay. That cost primarily falls on women who can spend upwards of $2,000 annually not to have a child.
A pathway forward for hormonal and non-hormonal male contraceptives has seen numerous false starts. These treatments often take aim at sperm maturation or spermatogenesis.
Hormonal male contraception methods usually indirectly suppress the levels of testosterone and spermatogenesis in the testes. However, playing with hormones is a surefire way to end up with side effects.
The dearth of male contraceptives on the market is partly due to a double standard. Health scientists end up looking hypocritical when complains of mood swings or acne halt male contraception studies. After all, these are the same side effects women have suffered with for decades.
Around 12% of women between 15 and 49 use an oral contraceptive as their birth control method. For them, the drug’s side effects are worth the alternative health outcome: unwanted pregnancy.
From another perspective, the success of a drug trial comes down to balancing physical health and benefits. The natural state of a sexually active man with no hormonal birth control is neutral, whereas the natural state of a sexually active women includes pregnancy. Thus, while the benefits for women far exceed the loss in physical health, the same can’t be said for males in these studies.
The research out of the Levin laboratory sidesteps the problem of hormonal side effects by targeting a sperm protein rather than spermiogenesis. To target sperm maturation, past hormonal and non-hormonal treatments usually involved months of daily applications before and after induced infertility. The new approach presented by the Levin laboratory in their Balbach et al. paper involves a single dose for immediate and quickly reversible contraception.
There is a hormonal method of male contraception coming down the clinical pipeline. Around 420 couples are currently taking part in phase 2 clinical trials for a topical gel that combines the drugs Nestorone and Testosterone. The trial is predicted to conclude by 2025, but previous delays raise skepticism.
The protein targeted in the Levin laboratory is called soluble adenylyl cyclase or sAC. After mature sperm are stored in the male epididymis, a chemical reaction is responsible for getting their tails wagging. Combining with the other seminal fluids and introduction to the vaginal canal exposes sperm to high concentrations of bicarbonate. This exposure triggers a chemical cascade initiated by sAC, activating motility and preparing sperm cells for fusing with the egg.
Scientists know that sAC mutations lead to immobile sperm and a few minor phenotypes, such as elevated intraocular pressure and kidney stones. Using a high throughput screen, Balbach et al. found a non-toxic allosteric inhibitor of sAC. Then using structure-assisted drug design, they developed several potent sAC inhibitors with drug-like properties. The laboratory then used the semen of male mice and humans to test in vitro applications. The researchers determined if this treatment affected the health or behavior of the mice.
After seeing no negative health impacts after six weeks of continual use of the sAC inhibitor, Balbach et al. predict transient blocking of sAC can avoid these side effects.
Forty years ago, it didn’t look like male contraceptive drugs would be necessary. A procedure called reversible inhibition of sperm under guidance or RISUG was described as “the IUD for men.” This gel treatment requires a trip to the doctor’s office for an injection rather than the scalpel necessary for a vasectomy. During a 10-minute procedure, a glue-like hydrogel is injected along the vas deferens, allowing fluid passage but not sperm from the testes. Yet, RISUG seems to be languishing in phase 3 of India’s clinical trial process for unreported reasons.
Pharmaceutical companies could doubt that RISUG has a long enough shelf life to please the FDA. A slightly different version of physical inhibition called Vasalgel became a new focus. It was initially touted to be approved by 2020 but is now predicted to come to market in 2024. Alternatively, in November of 2022, a medical company called Contraline touted the first implant of their flagship product, a hydrogel implant called ADAM, set to complete its study in 2025.
If all goes to plan, these gels will have limited time on the market before the TDI-11861 prototype is developed and released. This inhibitor demonstrated a magical combination of low levels of cross-reactivity with off-target enzymes and high binding affinity with sAC. TDI-11861 was safe and effective in vitro and spent a long time attached to the sAC protein, even under conditions mimicking the dilution experienced in the female reproductive system.
The dosed male mice and their female mates demonstrated no long-term damage to organs or cytotoxicity. The treatment did not affect male mouse sexual behavior or ejaculation.
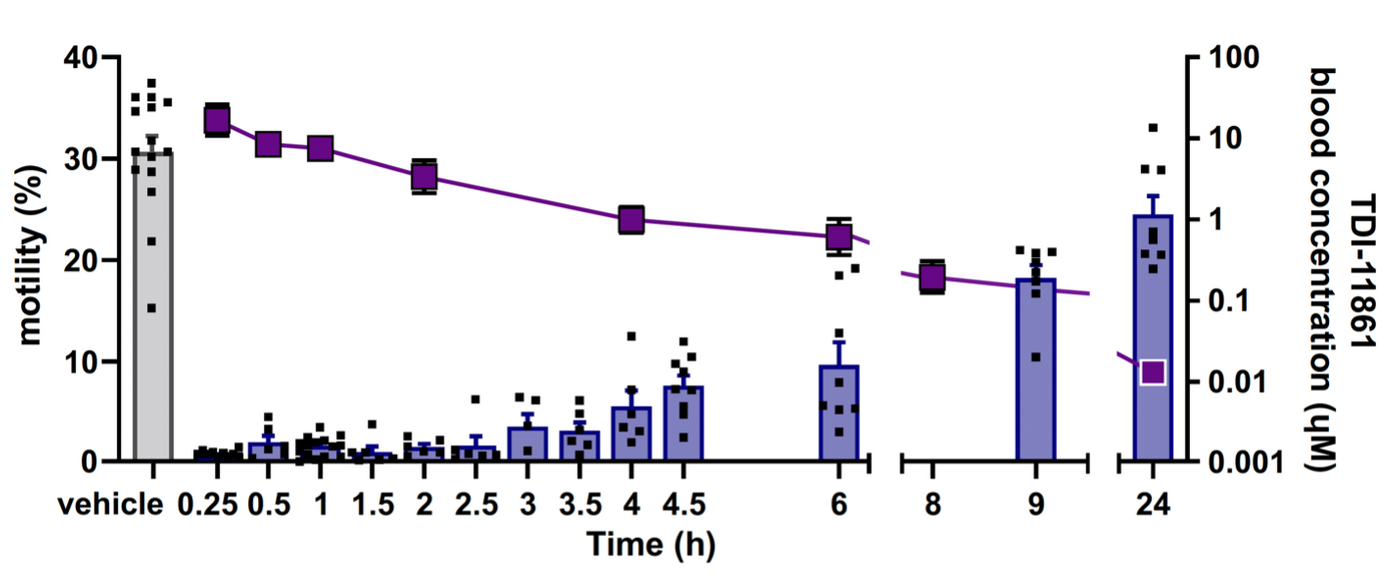
Perhaps the most significant selling point is the rapid and temporary nature of TDI-11861’s sperm inactivation. First author Dr. Balbach explains that "our inhibitor works within 30 minutes to an hour. Every other experimental hormonal or nonhormonal male contraceptive takes weeks to bring sperm count down or render them unable to fertilize eggs." Dosed male mice were infertile from 0.5 to 2.5 hours post-injection. If this proof-of-concept pans out, a single oral or injection of their inhibitor will block sperm mobility for up to 2.5 hours.
Image Credit Levin Laboratory of Weill Cornell Medicine 2023, via Creative Commons license CC BY 4.0, no alterations made.
Twenty-four hours after injection with the prototype, newly released sperm had regular motility. This treatment might offer a highly reversible state of sterilization.
The authors predict that the impeded sperm will remain trapped in human female vaginas, unable to enter the cervix with impaired mobility. As the vaginal canal transitions back to its default pH, the remaining sperm will be no more.
The authors tout their discovery as both non-hormonal male contraception and on-demand pharmacological contraception. Unlike an immobile sperm, this research might have the potential to go the distance.
Sources: Nature Communications, CDC, Vice, Life Sciences Intelligence, Contraline, Basic and Clinical Andrology, USA Today, Indian Journal of Urology, The United Nations World Population Prospects