How much medication should you be prescribed? Everyone is born with a different body, so how much and what kind of medication needs to be tailored to you.
For instance, after a patient has received an organ transplant, they are at risk of their body rejecting the new organ. To combat this, doctors heavily treat the patient using immunosuppressive drugs.
Immunosuppressive drugs have a narrow therapeutic range. If the dose is too high, it is toxic. If the dose is too low, it could fail to keep the body from rejecting the organ. Clinicians keep a close eye on their patients and make decisions about adjusting the dose according to how they are responding the drugs. They additionally decide whether the patient needs additional medications or therapies, such as dialysis. They ultimately consider a plethora of factors before deciding on their patient’s prescription regime.
But, when it comes down to it, those “decisions” are actually educated guesses. Doctors can’t be 100 percent sure how a patient’s body will react. After all, a patient’s ethnicity, age, genetics, and comorbidity all affect how they respond to a medication.
Now, a pilot study has demonstrated the effectiveness of a computational tool that could take the guesswork out of prescribing medications for immunosuppression, cancer, heart disease, bacterial infections, and other conditions that require tightly controlled treatment regimens. The research was published on April 6, 2016, in the journal
Science Translational Medicine.
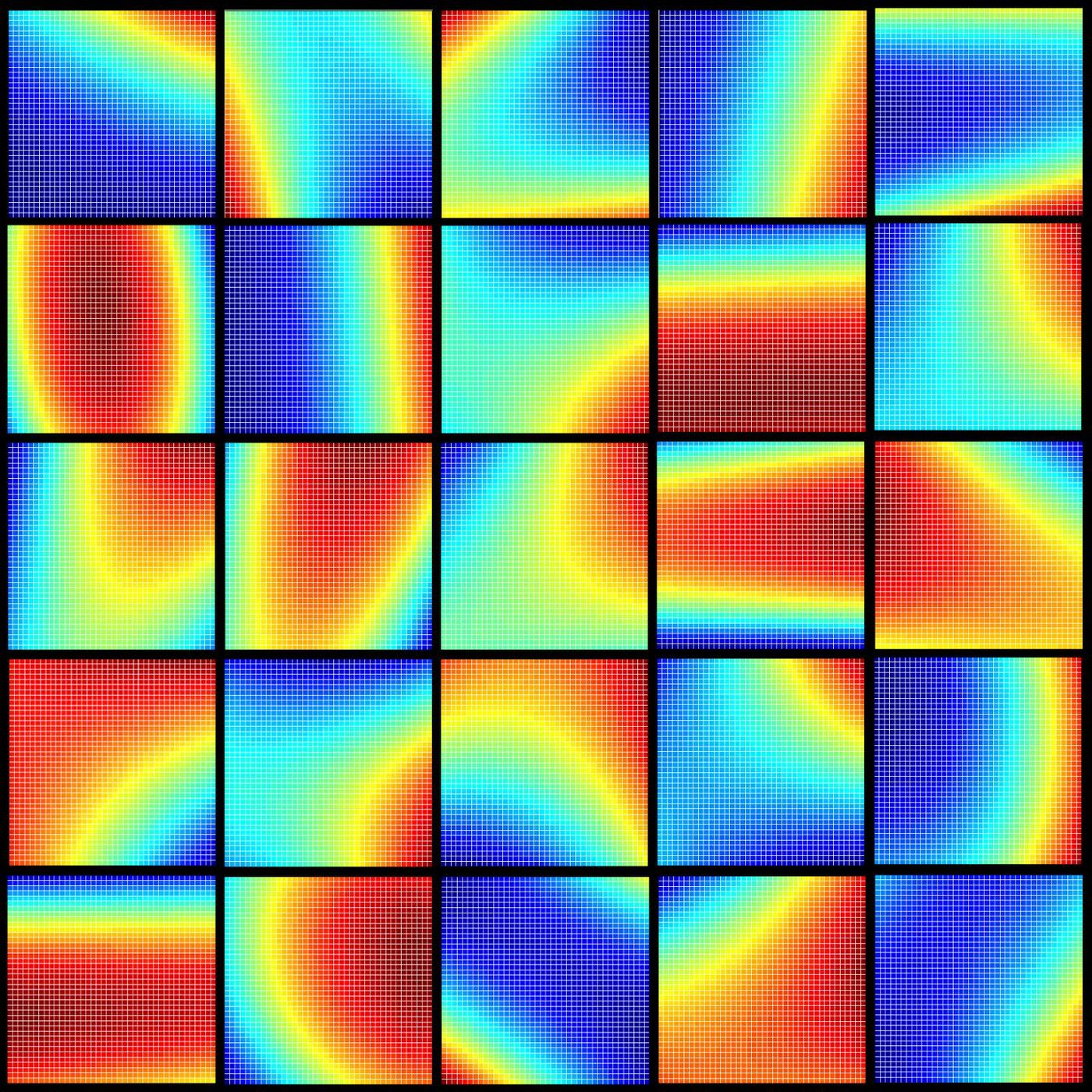
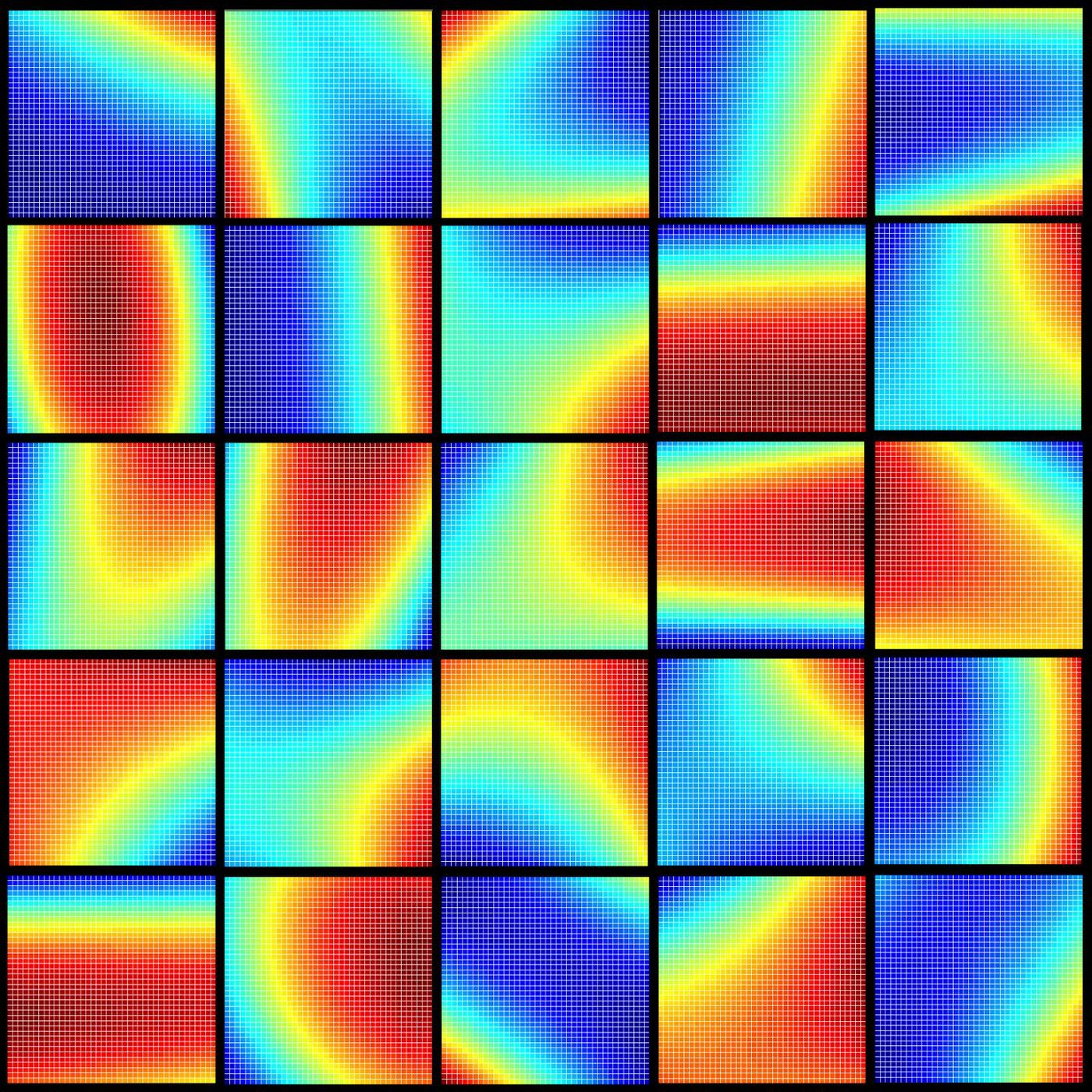
The tool, called parabolic personalized dosing (PPD), uses a mathematical approach to predict the next best dose of a drug for an individual. It harnesses a patient’s clinical data, such as the drug concentration in the bloodstream, to predict the next ideal dose per patient. PPD is different from other approaches based on mathematical modeling in that it uses an algebraic equation to build a parabolic map of the patient’s response to a drug.
In the pilot trial, UCLA researchers treated four liver transplant patients with immunosuppressant drugs using doses determined by PPD. Another group was prescribed immunosuppressant drugs using standard physician-guided dosing. The patients guided by PPD stayed within the target drug dosing range more frequently than the latter group. The PPD patients also tended to have shorter hospital stays.
The trial showed PPD also has the potential to optimize dosing for patients using a combination of drugs. The researchers hope clinicians will use PPD in the future to automatically tailor drug dosing for a wide range of patients, including those with cancer and heart disease.