Vitamin A Gives Immune System Power to Fight Tuberculosis
Multidrug-resistant tuberculosis bacteria are a serious health concern for the global population, but a new finding offers a new therapeutic solution that may be impervious to the development of resistance: vitamin A.
From Trinity College Dublin, scientists show how vitamin A supports the lung immune system in the fight against tuberculosis (TB), indicating a new type of immunotherapy that could help treat the disease, which killed 1.7 million people in 2016. TB is considered to be the leading cause of death from infectious disease across the globe.
A bacterial infection caused by the organism Mycobacterium tuberculosis, TB usually involves the lungs, but bacteria can invade the kidney, spine, brain, and other organs. A TB infection can be latent, causing no symptoms, but the infected person can still pass on the disease to someone else, whose immune system may not be strong enough to prevent a full-on TB infection.
Symptoms of such an infection include bad cough, chest pain, and coughing up blood or phlegm from deep in the lungs. The Bacille Calmette-Guerin vaccine prevents TB infection (although not 100 percent of the time), and it is often used in infants and young children in countries outside of the United States. Multiple-drug resistant strains of TB are particularly dangerous, as physicians are either forced to use harsh drugs that harm the patient while treating the infection or run out of therapeutic options completely.
Interestingly, vitamin A deficiency is relatively common in TB patients, and people with this deficiency are ten times as likely to develop the disease. Needless to say, vitamin A soon became the main topic of many studies.
Vitamin A is known for its role in immune function, vision, reproduction, and cellular communication. It’s found in dairy products, fish, meat, and other animal sources.
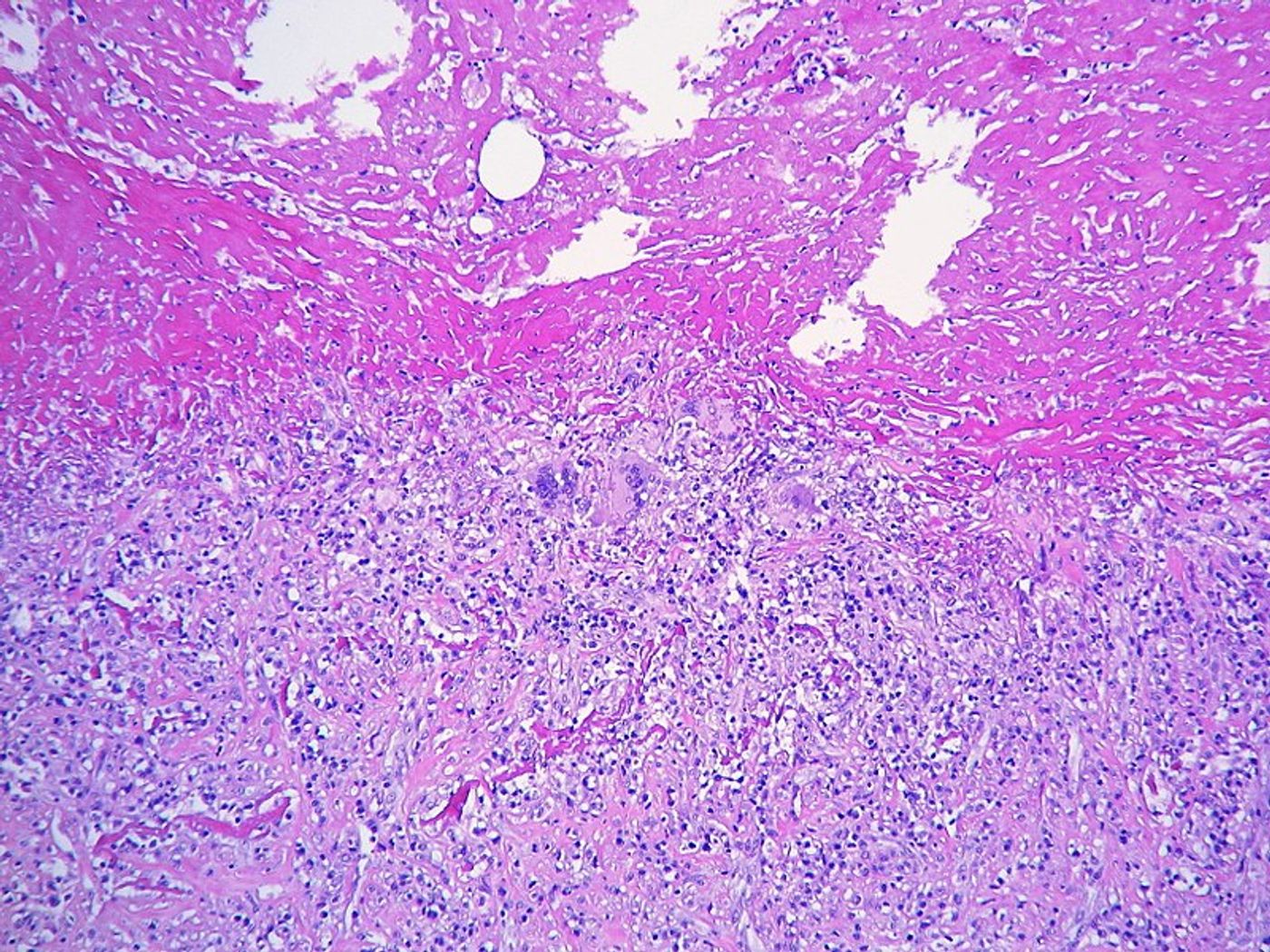
In the new study, researchers investigated the relationship between vitamin A and the immune system during TB infection. They found that increased vitamin A consumption greatly improves an immune process called autophagy. Fulfilled mostly by phagocytic cells like macrophages, autophagy consists of breaking down and recycling dead and dying cells, cellular debris, and pathogens. This is all through a process called phagocytosis, where cells engulf and break down the object of destruction.
Additionally, researchers found that vitamin A consumption enhances the phagocytic activity of macrophages during a TB infection. Paired with the finding from a past study that vitamin A also promotes anti-inflammatory activity, researchers were assured that they were onto something.
“TB remains a pressing global issue affecting millions worldwide. The high prevalence of vitamin A deficiency is a major driver in the global TB epidemic,” concluded lead author Dr. Sharee Basdeo Trinity. “Our next step will be to translate our research from the laboratory bench to the bedside. If this works out, we would plan to add vitamin A to the existing drug therapies to improve the outcome for our patients."
The present study was published in the American Journal of Respiratory Cell and Molecular Biology.
Sources: Centers for Disease Control and Prevention, National Institutes of Health Office of Dietary Supplements, Trinity College Dublin