Exciting new ideas to combat cancer are being developed every day across the field of oncology. One promising avenue is to make use of the immune system, enhancing it so that it may identify, seek out, and destroy cancer cells just like it does with other threats that arise from outside of the body. Cancer is a disease that can elude the immune system so well because it originates within the body and can go undetected due to its similarity to other innate cells. With the identification of neoantigens, however, scientists hope to make use of them to develop vaccines for cancer.
A new study conducted at the Biodesign Institute of Arizona State University by a team of researchers including Stephen Albert Johnston was published in the journal Scientific Reports, detailing a method for pinpointing tumor-specific factors in the blood that can elicit a protective immune response in the body which can be used to create effective cancer vaccines.
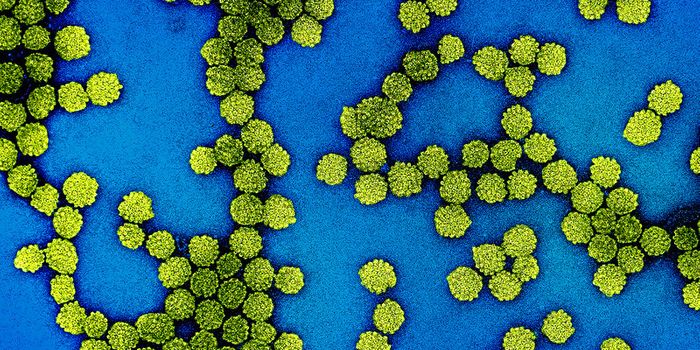
The team of scientists makes use of blood samples and established libraries of peptides arrays on a pre-loaded slide to identify which cancer neoantigens from the blood have an immune reaction to antibodies. If the antibodies react with the neoantigens, it would suggest they are recognized by the immune system and may be used in a vaccine against that cancer.
The researchers share that the results mean tumor-associated peptide mutations not only bind with immune antibodies but can effectively provide cancer protection — the team utilized animal models to prove the efficacy. Dog models with various forms of cancers similar to those seen in humans were used to provide blood samples. The peptide array and antibody technology provided the identification of which neoantigens might solicit the highest level of protection when used to develop a cancer vaccine. Once the mutated peptides with the most immune response were chosen, the vaccine was used on mouse models.
Johnston and his colleagues used peptide arrays to screen for tumor-linked peptides in blood samples from dogs, examining responses to 9 different forms of cancer. The antigens showing the most significant immune response in the array were then evaluated for their protective effect against two types of cancer, in a mouse model.
The study confirmed that some of the peptides exhibiting a strong antibody response on the peptide arrays offered protection from cancer in mice, while non-immunogenic peptides did not.
"Our system has the advantages of not requiring tumor tissue to DNA sequence and not having to guess whether a mutation elicits an immune response," Johnston says.
In their study, the scientists describe how the tumor-specific peptides are identified when looking at a frameshift mutation specifically. A frameshift mutation is a genetic mutation caused by a deletion or insertion of NDA sequence that shifts the way the sequence is read. A DNA sequence is a chain of many smaller molecules called nucleotides.
Further analysis of the frameshift mutated peptides provides insight that those with the highest immune reaction also provide T cells protection from cancer in mice. Those mutated peptides with the little or no immune reaction did not protect a vaccine.
The team hopes their research will pave the way for future effective cancer vaccinations as well as less intrusive ways to determine cancer neoantigens. Harnessing the power of the immune system to battle disease continues to offer much promise.
Sources: Scientific Reports, Science Daily, YouTube