Neuroscience
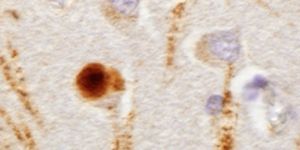
Penn Study Describes New Models To Test Immune-based Drugs for Parkinson's Disease
 Necessity is the mother of invention and that's what happened in the Soviet Union when they didn't have access to leading edge antibiotics that were developed in the West. Instead, the Soviet medical establishment relied heavily on bacteriophages - viruses that kill bacteria. Known as "phage therapy" this approach never caught on elsewhere, but is still used in Russia, Georgia, and Poland.
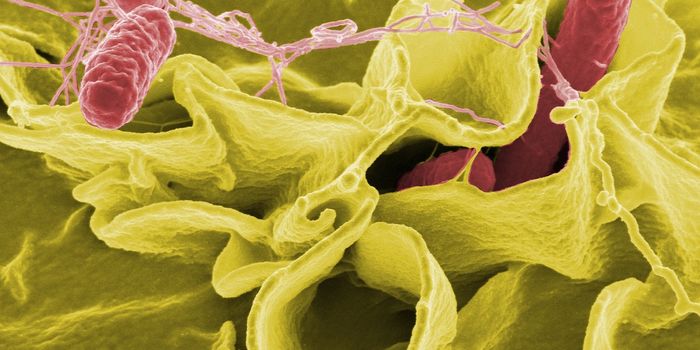
Necessity is the mother of invention and that's what happened in the Soviet Union when they didn't have access to leading edge antibiotics that were developed in the West. Instead, the Soviet medical establishment relied heavily on bacteriophages - viruses that kill bacteria. Known as "phage therapy" this approach never caught on elsewhere, but is still used in Russia, Georgia, and Poland.The start of phage therapy goes back thousands of years when people noticed that some river water could cure diseases such as leprosy and cholera. By the 20th century scientists figured out that it was because the water harbored certain viruses which killed certain bacteria. In the 1920's researchers in both the U.S. and Soviet Georgia began developing and using bacteriophages. But, in the 1940's doctors in the West started to turn more and more to powerful antibiotics and never looked back.
Western doctors got used to treating unknown infections with broad-spectrum antibiotics. Phages kill just once species or strain. We now know that broad-spectrum approach leads to resistance and is self-defeating in the long run. There is also growing acknowledgement that killing beneficial bacteria along with the harmful ones creates and environment where antibiotic-resistant bacteria can flourish. Being highly species-specific, phage therapy is unlikely to affect a patient's good bacteria. Due to this specificity if it is not known what species of bacteria is causing an infection, a cocktail of different phages must be made to fight it. But, there is an almost infinite supply of different phages, so if a bug develops resistance to one type of phage, different phages can be mixed into the cocktail.
Now, another necessity may make phage therapy more popular in the West as researchers look for ways to get around the growing problem of antibiotic resistance. The US National Institute of Allergy and Infectious Diseases currently lists phage therapy as a part of its plan to fight antibiotic resistance. In 2010 Texas A&M University set up the Center for Phage Technology, which due to lower regulatory barriers concentrates only on animal and plant applications. And, the European Commission is planning to fund Phagoburn, a large-scale clinical trial of phage therapy. 220 burn victims whose wounds have become infected with Escherichia coli or Pseudomonas aeruginosa will be given phage preparations and studied.
Although governments are expressing more interest in phages, pharmaceutical companies, for the most part, are not following along. Why not? Money, of course. Phases occur naturally and their use goes back for almost 100 years, so it is unlikely a drug company would be able to patent a phage therapy. But, there is hope that precise combinations of phages that target specific bacteria could be patented. Also, at a recent meeting of the American Society of Microbiology a paper was presented that presented work on a genetically engineered phage. The results of the research were promising and it's thought that such engineered phases could theoretically be patented.
Nothing is completely safe, and there is the possibility that phage therapy could adversely impact non-target tissue and non-target microbiota, but as currently practiced, phage therapy rarely causes more than minor side effects. In a 2011 paper entitled, Phage Treatment of Human Infections, that looked at the history of phage therapy, how it works, and its safety, authors Stephen T. Abedon, Sarah J. Kuhl, Bob G. Blasdel, and Elizabeth Martin Kutter conclude, "Phage therapy has a long history, though for most of that history this approach has been neglected by the English-speaking western world. We show here, however, that there is much more in the literature than has generally been realized, with many studies demonstrating that phages as natural and self-amplifying antibacterial "drugs" could be used to safely and effectively treat or prevent many common human diseases of bacterial etiology."
You May Also Like
DEC 19, 2024
Cell & Molecular Biology
A new study has shown that people who have asthma or sniffling caused by allergies also carry a different set of fungi i
...
Written By:
Carmen Leitch
DEC 30, 2024
Cell & Molecular Biology
RNA in cells performs an astounding number of functions. Messenger RNA carries the sequences of active genes to the cell
...
Written By:
Carmen Leitch
JAN 14, 2025
Clinical & Molecular DX
Worldwide, asthma is the most common chronic respiratory illness that affects children, particularly Puerto Rican and Bl
...
Written By:
Carmen Leitch
FEB 19, 2025
eBooks
The rise of antimicrobial resistance and novel emerging diseases has put microbiology at the forefront of public percept
...
Sponsored By:
BMG LABTECH
JAN 30, 2025
Immunology
Since the inauguration of President Donald Trump on January 20th, 2025, he has signed many executive orders, changing po
...
Written By:
Brian G. Morreale
APR 10, 2025
Immunology
The immune system works to maintain homeostasis throughout the body. Various cell types and immune mechanisms work in co
...
Written By:
Brian G. Morreale
Loading Comments...