Scientists from the Beth Israel Deaconess Medical Center (BIDMC) have been studying immune action in cases of inflammatory bowel disease (IBD) for more than ten years. This week, they discovered a connection between immune cells and cytokine signaling that could change the way people live with IBD.
According to the
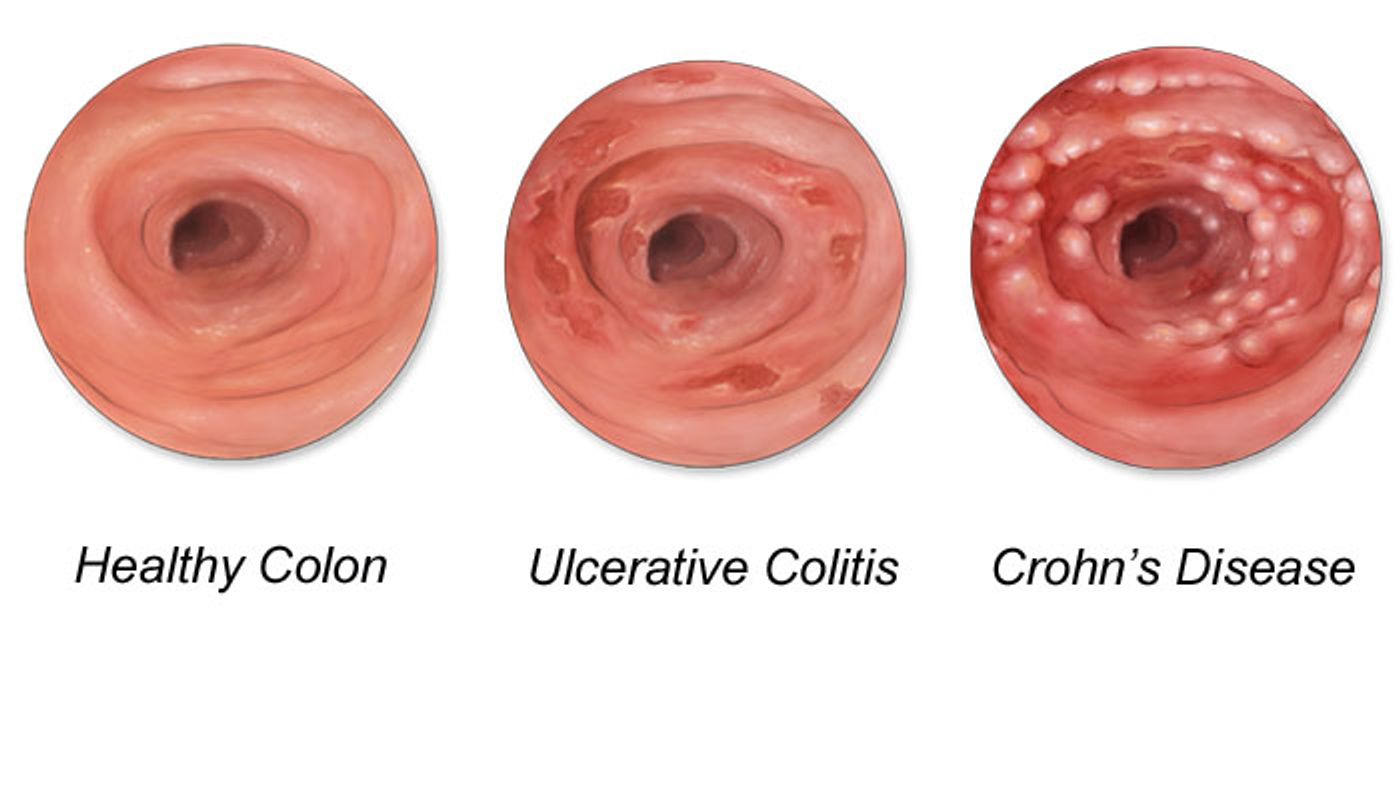
CDC, common types of IBD like Crohn's disease and ulcerative colitis affect more than a million Americans. These diseases are characterized by chronic inflammation of the gastrointestinal (GI) tract due to an unwarranted immune response. The immune cells act as if normal compounds in the GI tract are foreign and dangerous.
The basic premise of IBD involves the unregulated action of effector immune cells in the GI tract; cytokines are released and stimulate inflammation of the bowels even though no pathogens or damages are present. The scientists from the BIDMC study the two immune cells involved in the troubling IBD immune response: CD4 T cells and Type 1 CD8+ T cells (T
C1).
Specifically in Crohn's disease, T
C1 cells produce interferon gamma, a cytokine that induces inflammation. Normally, regulatory immune cells inhibit the action of T
C1 cells when no action is required, but Crohn's disease patients are chronically unable to perform this maintainence. To make up for this malfunction, the scientists looked at the expression of CD39, an ectoenzyme, on T
C1 to see if they could halt the overproduction of interferon gamma.
Ectoenzymes like CD39 have their enzymatically active site outside the plasma membrane, in the extracellular environment. CD39 is naturally expressed by dendritic cells and some regulatory cells and acts as an immunosuppressive.
CD39 is able to regulate the autoimmune reactions in Crohn's disease through "catalytic conversion of proinflammatory extracelluar ATP to immunosuppressive nucleosides" like adenoside, a behavior used by the BIDMC scientists over the past decade as they looked for a way to counter the effect of IBD. Essentially, this enzyme transforms the energy produced by the GI tract inflammation into a product that suppresses the inflammation.
To conclude their study, the scientists from BIDMC were able to put all of the pieces together by discovering that upregulation of CD39 in IBD patients helped suppress and inhibit interferon gamma production in neighboring T
C1 cells. This connection leads to promising new treatment plans for IBD patients, manipulating the body's natural way of controlling inflammation.
Check out the video below to learn more about Crohn's disease and how inflammation of the GI tract affects digestion.
Source:
Medical Xpress