COVID Cytokine Storm Chasers Look Inside the Lungs
Immunologists have revealed one of the underlying mechanisms behind COVID’s life-threatening cytokine storms. By studying ventilated patients battling severe forms of COVID, they attributed systemic inflammation to the immune system’s overzealous attempt to eradicate the virus from the lungs. The study was published in Immunity.
Patients with severe COVID-19 infections require ventilation because their lungs are damaged, limiting their ability to take in oxygen. Once they reach this critical stage of disease progression, the risk of mortality is around 40 percent.
To better serve these at-risk patients, researchers have been hunting for how the immune system influences this rapid deterioration, such that they can develop treatments to address it. However, very few studies have taken a closer look at immune activity inside the respiratory tract—most of them examine immunological markers in the blood.
Much like storm chasers, a team of scientists studied patients’ lungs—right where the immune hurricane begins brewing—to uncover the true nature of COVID cytokine storms. Professor Donna Farber and colleagues from Columbia University’s Irving Medical Center obtained saline washes from ventilator tubes used by COVID patients in ICU, which contained trace numbers of respiratory immune cells. As part of their investigation, they collected and analyzed both saline wash samples and blood samples from 15 ventilated COVID patients.
"It seems obvious that the immune response in the respiratory tract would drive a disease caused by a respiratory virus, but we didn't know what the processes were and how they worked together with systematic responses," Farber said.
"What's new here is that we've been able to simultaneously sample both the respiratory tract and the blood over time and put together a more complete picture of the responses involved and how local and systemic responses work together."
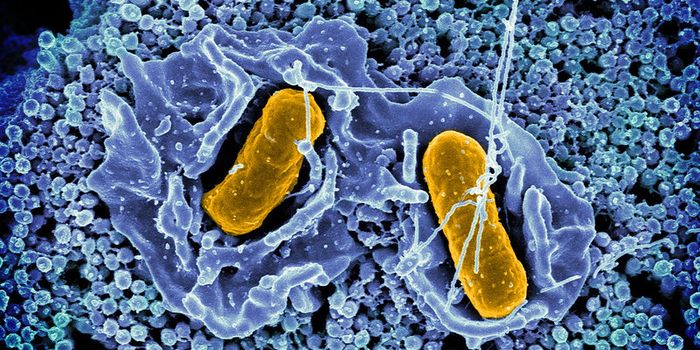
Farber’s team found that CCL2 and CCL3 cytokines released by the lung played a central role in aggravating COVID symptoms. These immune factors channeled monocytes into the lungs, cells which don’t even belong in the respiratory system.
"Normally, these cells never make it to the airway, but in severe COVID patients, they accumulate throughout the lung and clog up the alveolar spaces," explained Farber.
Treatments to inhibit these cytokines hold the potential to quiet the cytokine storm and prevent long-term lung damage. One such CCL2 inhibitor is currently being investigated in a clinical trial.
Sources: Eurekalert, Immunity.