Bacteria in the Lungs Can Impact Immune Cells in the Brain
Research has revealed that nearly the entire human body has been colonized by microbes. While studies have shown just how closely we are connected to the microbes in the body, some of those connections are still surprising. For example, though small, there is a community of microbes in the lungs. While the composition and function of the lung microbiome is still under investigation, new research reported in Nature has revealed that there seems to be a close link between the lung microbiome and the brain.
The lung microbiome appears to influence the activity of immune cells in the brain called microglia. The lung microbiome can impact the risk of autoimmune inflammation in the brain. That type of inflammation has been observed in several diseases including multiple sclerosis.
Microbes in the lung appear to send signals to microglia in the brain, which can then react rapidly to threats, explained first study author Dr. Leon Hosang of the University Medical Center Göttingen.
"The lung microbiome can, therefore, be seen as an early warning system for the sensitive brain tissue," added co-senior study author Francesca Odoardi, Heisenberg Professor at University Medical Center Göttingen.
Many environmental influences could be affecting immunity in the brain this way, like lung infections, air pollution, or antibiotics that affect the lung microbiome, for example. Smoking is also known to increase the risk of multiple sclerosis, an autoimmune disorder. It may also be possible to target the lung-brain axis for therapeutic use.
"For example, a dosage of probiotics or specific antibiotics could be used to influence the brain's immune reaction in a targeted fashion in order to treat not only multiple sclerosis but also diseases of the central nervous system in general where the immune activity of microglia plays a role," suggested co-senior study author Alexander Flügel, a Professor at the University Medical Center Göttingen.
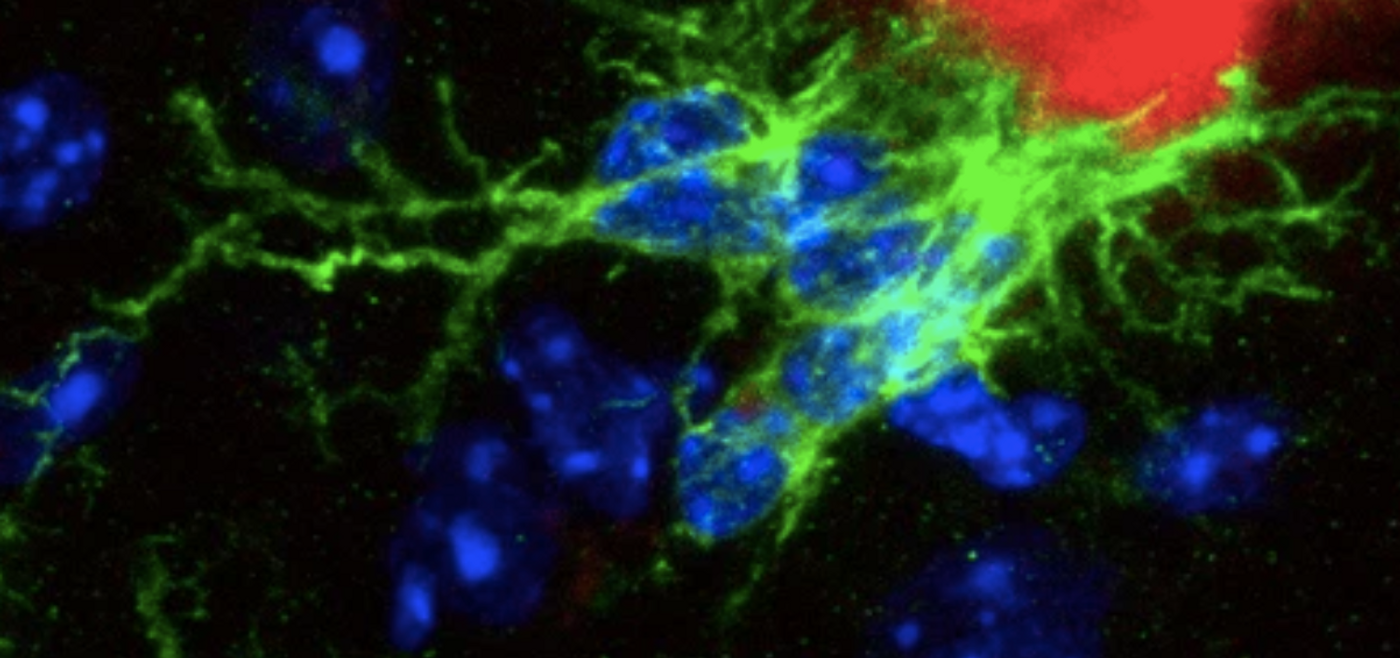
Although not many microbes can be found in the lungs, they seem to be sensitive to changes that occur. A local, low dose of antibiotics in a mouse model was enough to cause changes in the risk of autoimmune disease in the brain. When the researchers exposed the mouse lung microbiome to antibiotics, they found that microglia in the brain were then altered. Microglia have fine branches, and changes could be seen under a microscope. Those branches became shorter and thicker after the antibiotic treatment and the microglia had a weaker reaction to inflammatory signals. That drew fewer immune cells to the site of inflammation.
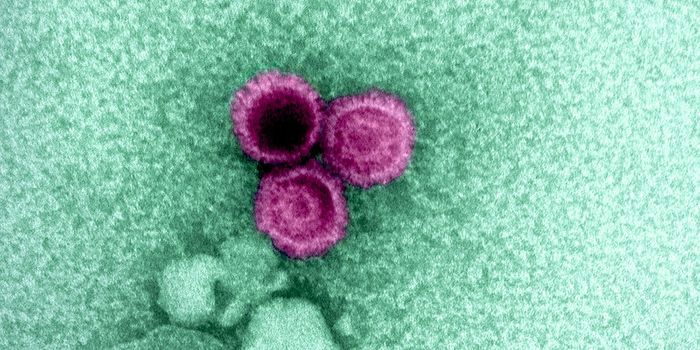
Bacteria in the lungs generate a molecule that makes up part of their cell wall, a lipopolysaccharide. This molecule began to build up in lung tissue after antibiotic exposure. The weak microglial response and autoimmune resistance were triggered by increased levels of lipopolysaccharide. When lipopolysaccharide levels in the lungs were reduced, however, the autoimmune disease got worse.
Sources: University Medical Center Göttingen, Nature