A Failed Immunotherapy Trial Leads to a Crucial Discovery
Immunotherapies, which boost a patient's immune system so it's better at fighting cancer, have been a game-changer in the world of cancer treatments. But immunotherapies are still not effective for most patients with solid tumors. In a recent clinical trial, scientists tested whether an immunotherapy regimen could help patients with head and neck cancer.
In cancer, there is often an excess of phosphoinositide 3-kinase (PI3K) activity, leading researchers to develop drugs that could tamp down that activity. The first such inhibitors were too broadly active, and induced a range of side effects. Currently, most PI3K inhibitors are meant to boost the production and activity of immune cells that fight cancer called CD8+ T cells, by acting on other cells called regulatory T cells that put the brakes on CD8+ T cells.
The Food and Drug Administration eventually approved a few drugs that inhibit the molecule more selectively, such as a breast cancer drug that acts on PI3Kα, and drugs that treat B cell malignancies by targeting PI3Kδ. Many of these drugs still carry the risk of serious side effects, however, and researchers were carefully monitoring a trial of PI3Kδ inhibitors meant to treat head and neck cancer patients.
"In the oncology world, immunotherapy has revolutionized the way we think about treatment," said co-study leader Professor Christian H. Ottensmeier, M.D., Ph.D., FRCP, of the University of Liverpool.
"Having an oral tablet that can take off the brakes - the T regs - can be a great asset for oncologists," said co-study leader Professor Pandurangan Vijayanand, M.D., Ph.D of the La Jolla Institute for Immunology.
In this trial, regulatory T cells that tamp down immune activity were suppressed as intended, and T cells that can fight cancer were able to access the tumors. However, the trial had to be halted for twelve of 21 volunteers because they were experiencing serious side effects; the patients were developing an inflammatory condition in the gut called colitis.
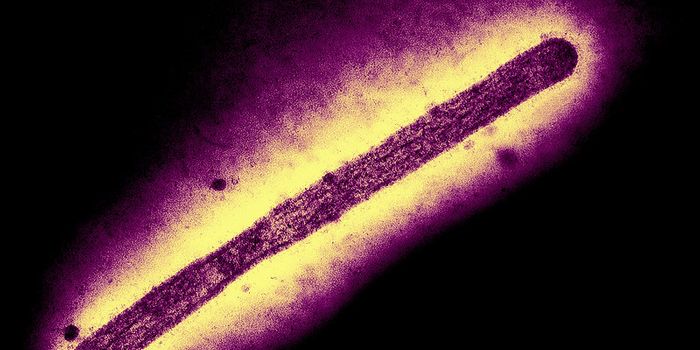
The researchers wanted to know what went wrong, so they analyzed immune cells from the patients. This revealed that while the PI3Kδ inhibitor increased tumor-fighting CD8+ T cells, it also interfered with the action of a very specific set of T cells that normally protect the gut. The investigators discovered that because those gut T cells were out of commission, disruptive Th17 and Tc17 cells could move in and cause inflammation there. The findings have been reported in Nature.
The scientists have hypothesized that a smaller dose of PI3Kδ inhibitor may now be able to effectively boost anti-tumor activity in the immune system, without having a detrimental impact on the gut. They are planning a new trial to test the lower dose, which could be effective against solid tumors, without causing adverse events that impact the immune system.
These adverse effects have not been seen in patients with other types of cancers that have been treated with PI3Kδ inhibitors; the researchers noted that in those patients, the immune system in the gut has already been compromised by previous cancer treatments.
Sources: La Jolla Institute for Immunology, Nature