An Antibody 'Decoy' Could Pave the Way for Better Immunotherapy
Immunotherapy called CAR T cell therapy is a treatment that aims to train immune cells to get better at fighting disease, typically some type of lymphoma. Many of these methods use a patient's own cells, and while they work well against some kinds of cancer, they are not very effective at destroying solid tumors. Therapies that are custom-made by harvesting a patient's own cells can be difficult and expensive to engineer. Therefore, cells that are mass-produced and can be broadly applied in CAR T cell therapy, so-called allogenic cells, will be important to develop so that CAR T cell therapy can be used on more patients.
One major challenge with allogenic cells is rejection. Just like a transplanted organ, the immune system of an allogenic cell recipient might reject those therapeutic, but generic and foreign cells. That rejection usually manifests as antibodies that bind to the foreign cells and neutralize their effect. Scientists may have found a way around this problem. Reporting in Nature Biotechnology, researchers developed a decoy that can catch those problematic antibodies, and remove them from circulation before the therapeutic cells are destroyed. The study authors also suggested that this method could work to improve the acceptance of organ transplants.
"This antibody-mediated rejection is really hard to overcome," said senior study author Tobias Deuse, MD, the Julien I.E. Hoffman, M.D. Chair in Cardiac Surgery at UCSF. "So, rather than trying to suppress the patient's immune system, we looked for ways we can alter the cells that the patient will receive and better enable them to survive."
Deuse added that allogenic CAR T cell therapy has been tested in clinical trials, and the outcomes have been worse than autologous CAR T cell therapy, which uses a patient's own cells. In immunotherapy, the therapeutic cells are also floating around in circulation, making them even more vulnerable to attacks from the immune system than if they were contained in a transplanted organ. These important cells have to be protected, said Deuse.
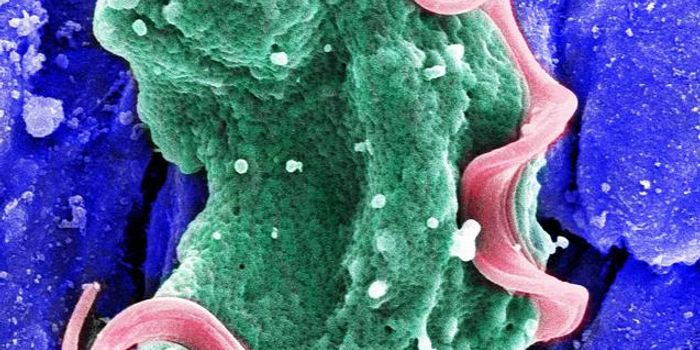
When antibodies bind to a target on a cell, it becomes a kind of beacon that signals to other immune cells, setting off a chain reaction that destroys the bound cell.
In this study, the investigators genetically engineered three cell types: CAR T cells, thyroid cells, and pancreatic islet cells that make insulin, to all display a receptor called CD64 on their surfaces. CD64 binds to antibodies that mediate immune rejection, so these engineered cells became decoys that captured the rejection antibodies, which were then prevented from activating immune cells.
"We saw that we can snatch up high levels of these antibodies, which resulted in very robust protection for the therapeutic cells," said Deuse. "This is clear proof-of-concept for this approach."
There are still major challenges to using these decoys, in part because they are still expensive and challenging to produce. The researchers are hopeful that this work will help lead to the development of allogenic cells that can be universally applied in a cost-effective way, so more patients can access them.
Sources: University of California, San Francisco (UCSF), Nature Biotechnology