A new study of gut bacteria in premature infants highlights the problem of antibiotic resistance and stresses how extremely vulnerable these young patients can be.
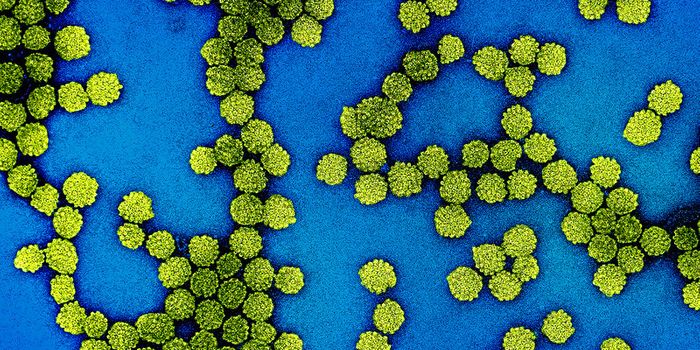
The gut microbiome has emerged in recent years as a vital player in human health, affecting nutritional status, bone development, and immune function. The new study warns that the microbes colonizing the gastrointestinal tracts of babies born prematurely are not health-promoting or even benign organisms, but close relatives of bacteria known to cause hospital-acquired infections, including Escherichia coli (E. coli), Klebsiella, and Enterobacter.
Researchers sequenced all of the DNA in the bacterial communities living in the preterm babies’ guts and identified almost 800 genes in these bacterial communities that confer resistance to antibiotics, about 80 percent of which had not previously been associated with antibiotic resistance.
“Our study demonstrates that even well-studied bacteria—the ones that we know cause disease or their close relatives—have many genes associated with antibiotic resistance that have not been characterized before,” says senior author Gautam Dantas, associate professor of pathology and immunology at Washington University in St. Louis. “Premature babies do not always get bacterial infections that need treatment, but we have known for a long time that they are at higher risk for infection than babies born full term. Now, we know that preterm infant guts are attracting exactly the wrong kinds of bacteria.”
Because of this increased risk of infection, almost all preterm infants cared for in neonatal intensive care units (NICUs) receive antibiotics in the first two days of life, regardless of their health status. And a majority of those receive many more days of treatment.
“Extremely preterm infants often have multiple medical problems, with symptoms of prematurity overlapping with other conditions like infection,” says coauthor Barbara B. Warner, professor of pediatrics and neonatologist at St. Louis Children’s Hospital. “The conventional wisdom has been antibiotics can’t hurt and they might help. But our new study demonstrates that wide-scale use of antibiotics in this population does not come without cost.”
The study, published in the journal
Nature Microbiology, included babies cared for in the NICU of St. Louis Children’s Hospital, where the investigators collected 401 fecal samples from 84 preterm infants over the first three months of life. Sequencing all the bacterial DNA in these fecal samples identified resistance genes to 16 different antibiotics.
The babies that received antibiotics only in the first few days of life served as a comparison group to the babies that received antibiotics early plus subsequent treatments later. On average, the babies that continued receiving antibiotics had a total of 21 days of treatment. All babies were born before 33 weeks’ gestation.
In general, the findings suggest it is better to have a high diversity of bacterial species living in the gut. Compared with babies born full term, preterm infants were found to have 10-fold fewer species of bacteria colonizing the gut. And among the preterm babies, those receiving the most antibiotics showed the least species diversity. Giving breast milk was associated with increased bacterial diversity, as was each baby’s increasing age, perhaps simply from having more time for exposure.
Collateral damage
The specific antibiotics associated with the lowest species richness were drugs called meropenem, cefotaxime, and ticarcillin-clavulanate. The meropenem finding is particularly alarming, Dantas says, because it’s part of the carbapenem class of drugs that are considered antibiotics of last resort. They are used to treat infections caused by bacteria closely related to the species most commonly found in these infants’ GI tracts.
“Consider what is going on in terms of selection pressure,” Dantas says. “As with any antibiotic, giving carbapenems encourages the selection of bacteria resistant to this drug. And if these microbes, which dominate these babies’ guts, become resistant to carbapenems, the microbes go on the highest urgency threat list at the Centers for Disease Control and Prevention.”
According to the CDC, carbapenem-resistant Enterobacteriaceae (CRE) are resistant to nearly all existing antibiotics and about half of patients in intensive care units who contract a bloodstream infection from CRE die from that infection. Enterobacteriaceae is a large family of bacteria that includes E. coli, Klebsiella, and Enterobacter.
In the new study, the two antibiotics most commonly given to the preterm infants were found to be vancomycin and gentamicin, which both had divergent effects on species richness. The researchers were able to predict the direction of this effect with high accuracy, based on the sequences of bacteria present and the resistance genes they carried in samples taken before treatment.
The findings also show that treating with one antibiotic can dial up resistance to seemingly unrelated antibiotics. This surprising finding makes sense because they found the majority of these microbes were resistant to multiple drugs, showing that resistance genes tend to cluster together in the same organisms.
“This data demonstrates the collateral damage these drugs can do,” Dantas says. “If doctors give penicillin, it makes sense that you will see enrichment in the proportion of bacteria resistant to penicillin. But perhaps a vancomycin-resistant gene is nearby. A doctor may not even be giving vancomycin, but vancomycin resistance increases because the genes happen to be grouped together.
“This is a consequence of our history of antibiotic use. We’ve given these bacteria powerful reasons to collect all these resistance genes together.”
The researchers hope that clinicians will use this information to make decisions about the best ways to treat these vulnerable patients.
“While antibiotics can certainly still be lifesaving, we are becoming more aware of the risks they pose,” Warner says. “This study arms us with information that may help us push toward shorter antibiotic treatment courses and minimizing the use of broad-spectrum antibiotics.”
Dantas expressed concern over the dwindling numbers of effective antibiotics and the fact that few new drugs are in development. He also suggested a shift in strategy for the design of new generations of antibiotics.
“If we can stop these bacteria from producing toxins, rather than kill them outright, we won’t see the same selection pressure,” he says. “We don’t necessarily need to kill these bacteria, we just need to stop them from killing us.”
The Children’s Discovery Institute, the March of Dimes Foundation, the National Institutes of Health, the Washington University School of Medicine through a Clinical and Translational Science Award (CTSA), the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and a Mr. and Mrs. Spencer T. Olin Fellowship funded the work.
Source:
Washington University in St. Louis
This article was originally published on
futurity.org.