There’s no cure for idiopathic pulmonary fibrosis (IPF), and the disease gets irreversibly worse as it progresses. As scientists frantically look for biomarkers to catch the disease early and begin treating symptoms, a new study shows that biomarkers for IPF may be the same as those for some types of cancer.
For people with IPF, usually older adults, their lung tissue becomes increasingly scarred over time. On average, people with IPF only live about three to five years after their diagnosis. Cause of death usually comes from respiratory failure, pulmonary hypertension, heart failure, pulmonary embolism, pneumonia, or lung cancer. Medical professionals believe that although the disease seems to be incurable, identifying patients as early as possible will give them the best chance of living longer and have a fuller life.
From the German Research Center for Environmental Health in a study published in the
European Respiratory Journal, scientists discovered a connection between myeloid-derived suppressor cells (MDSCs) in the blood and incidence of IPF. The higher the number of MDSCs, the more limited the lung function IPF patients had.
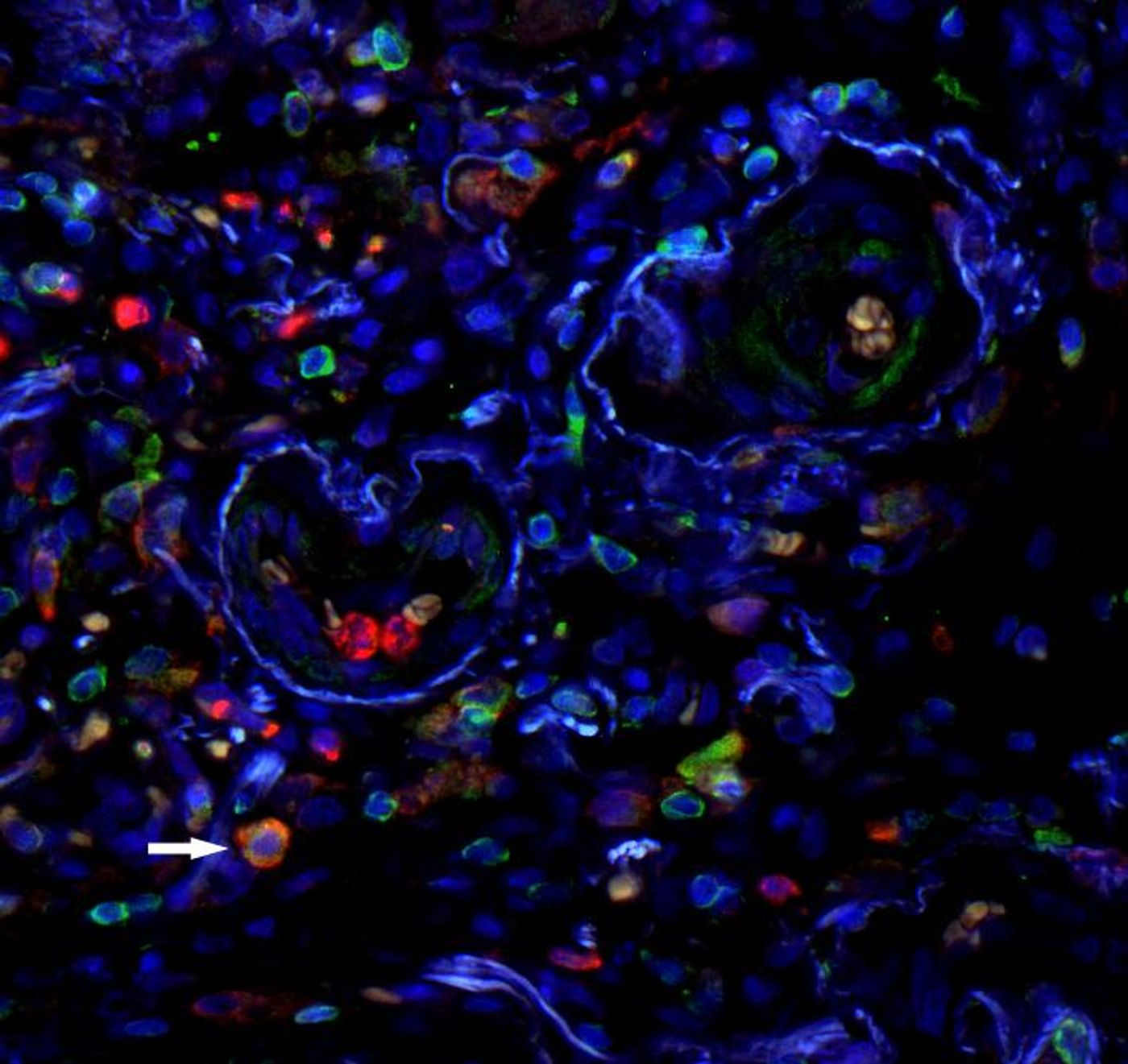
“MDSC are primarily found in fibrotic niches of IPF lungs characterized by increased interstitial tissue and scarring, that is, in regions where the disease is very pronounced,” said Professor Oliver Eickelberg, study leader.
MDSCs are capable of suppressing the T cell response, an ability that is helpful in regulating the immune response but not desirable in cases of cancer or infection. High levels of MDSC activity are known to contribute to a poor prognosis in certain instances of cancer, and Eickelberg’s team seemed to be on the verge of discovering a similar contribution in cases of IPF.
Eickelberg and his team looked at blood samples of 170 study participants, with almost half being IPF patients. They analyzed the samples, looking for lymphocytes like MDSCs that could be linked to IPF in some way. After successfully identifying a significantly higher count of MDSCs in IPF patients versus health control patients, the researchers also saw an inverse relationship existing between lung function and levels of circulating MDSCs. However, the relationship appears to be unique to IPF patients; no inverse correlation was found in patients with chronic obstructive pulmonary disease (COPD) or other interstitial lung diseases.
The researchers also measured gene activity common in immune cells, and found that immune-associated genes were expressed less frequently in blood samples with high levels of MDSCs. Observing human lung tissue from IPF patients also provided evidence supporting their claim that MDSCs were compromising the immune system, exacerbating cases of IPF.
Next, the team plans to determine how the presence of MDSCs in high quantities in the blood can be used as a biomarker for IPF, looking at how soon IPF could be diagnosed based on MDSC presence. Additionally, researchers will explore the possibility of suppressing accumulation of MDSCs as a potential treatment option for IPF.
Sources:
National Heart, Lung, and Blood Institute,
Nature Reviews Immunology,
Helmholtz Zentrum München