Red Blood Cells Equipped to Carry Autoimmune Disease Treatments
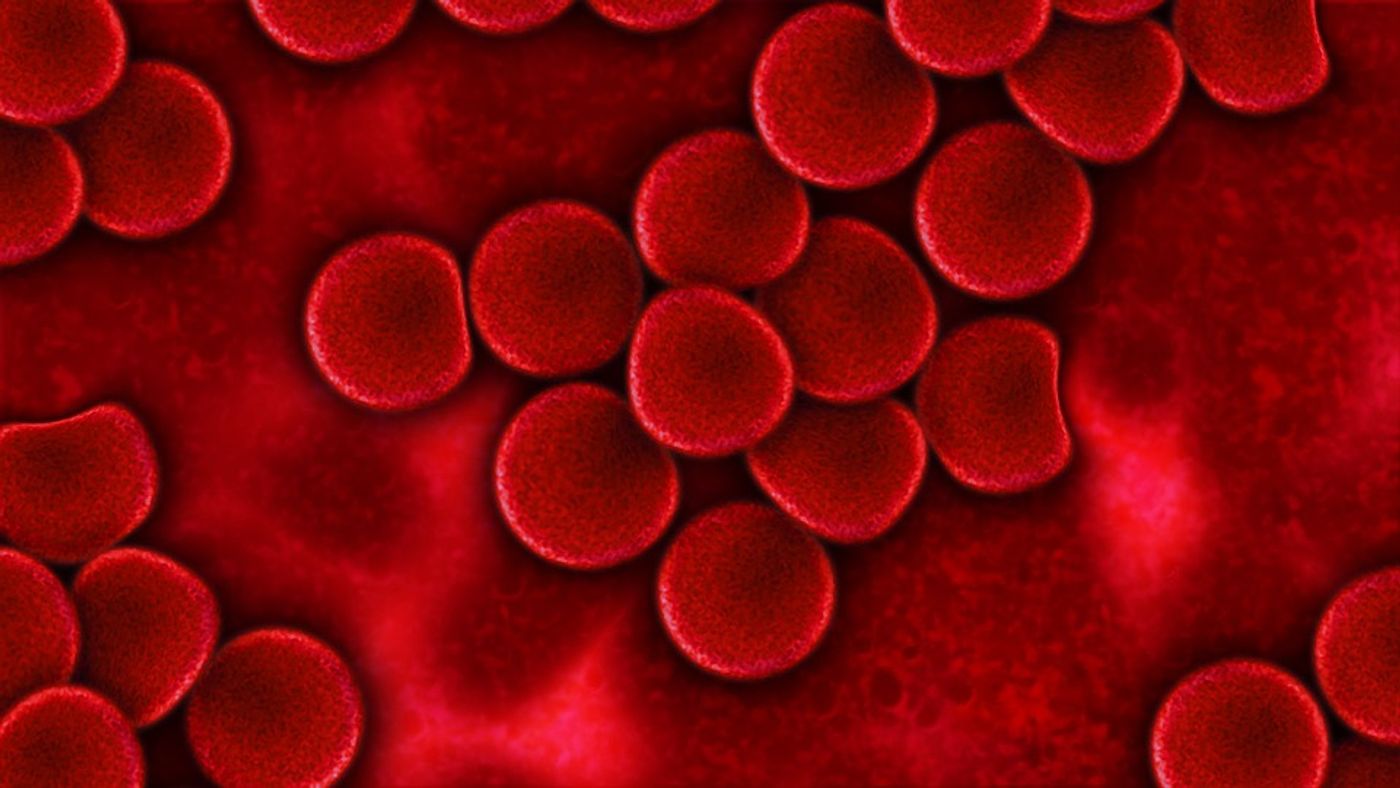
Researchers are “hijacking” red blood cells because of their ability to flow freely in and out of nearly all types of body tissues without being noticed by the immune system. By attaching proteins to the red blood cell surface, a team from the Whitehead Institute of Biomedical Research developed a new technique for desensitizing the immune system.
Autoimmune diseases like rheumatoid arthritis, multiple sclerosis (MS), and type 1 diabetes occur because of the immune system’s reaction to certain proteins as if they were foreign antigens, substances produced by pathogens that stimulate an immune response. However, in a new study published in the journal Proceedings of the National Academy of Sciences, researchers worked with red blood cells to suppress the immune response to these harmless proteins.
"Essentially what we're doing is hijacking the red blood cell clearance pathway, such that the foreign antigen masquerades as the red blood cells' own, such that these antigens are being tolerated in the process," explained MIT graduate student Novalia Pishesha.
Immunosuppressants are the typical option used to treat autoimmune diseases, which the National Institutes of Health estimate influence the lives of more than 23 million Americans. Immunosuppressants successfully regulate the immune response but also make an individual especially prone to infections. The new approach presents a new way to avoid the infection vulnerability: tolerance induction.
Tolerance induction involves taking peptides from antigens as a way to “retrain” the immune system to know when and when not to react. However, delivering the antigenic peptides to where they need to go without being attacked by the immune system poses a serious problem.
Scientists from the Whitehead Institute of Biomedical Research, during their study of red blood cells as potential vessels for carrying antigenic peptides, quickly saw the benefits of using these cells to carry immune-sensitizing proteins. Red blood cells regularly access nearly every type of tissue in the body, and they are recycled regularly without triggering an immune response against them.
Previous research from the same group involved tagging red blood cells with biotin, a B vitamin, and antibodies, via a technique called “sortagging.” Their present study involved early stage mouse models of autoimmune disease. They paired a sample of blood cells with antigens that prompt MS and type 1 diabetes and then transfused the cells back into the mice models. The process takes less than an hour, and researchers saw an immediate reduction in disease symptoms and prevention of further symptoms.
"If this type of response is also true in humans, then it could make a lot of these therapies possible for these diseases and similar conditions,” said MIT Professor Harvey Lodish.