Temporarily Muting Immune Regulation Focuses Attention on Cancer
The same immune process that protects the immune system from friendly fire by soothing inflammatory reactions and reducing numbers of “fighter” immune cells ironically ends up backfiring in many cases of cancer. A new way to kill tumor cells involves temporarily inhibiting this protective mechanism, so all hands are on deck.
Regulatory T cells, or Tregs, are designed to inhibit the immune response when an infection is under control or when the body mistakenly targets its own cells, preventing excessive inflammation and autoimmune diseases. However, Tregs also unknowingly prevent the immune system from using its full potential in the attack against cancer, and tumor cells take advantage of this error.
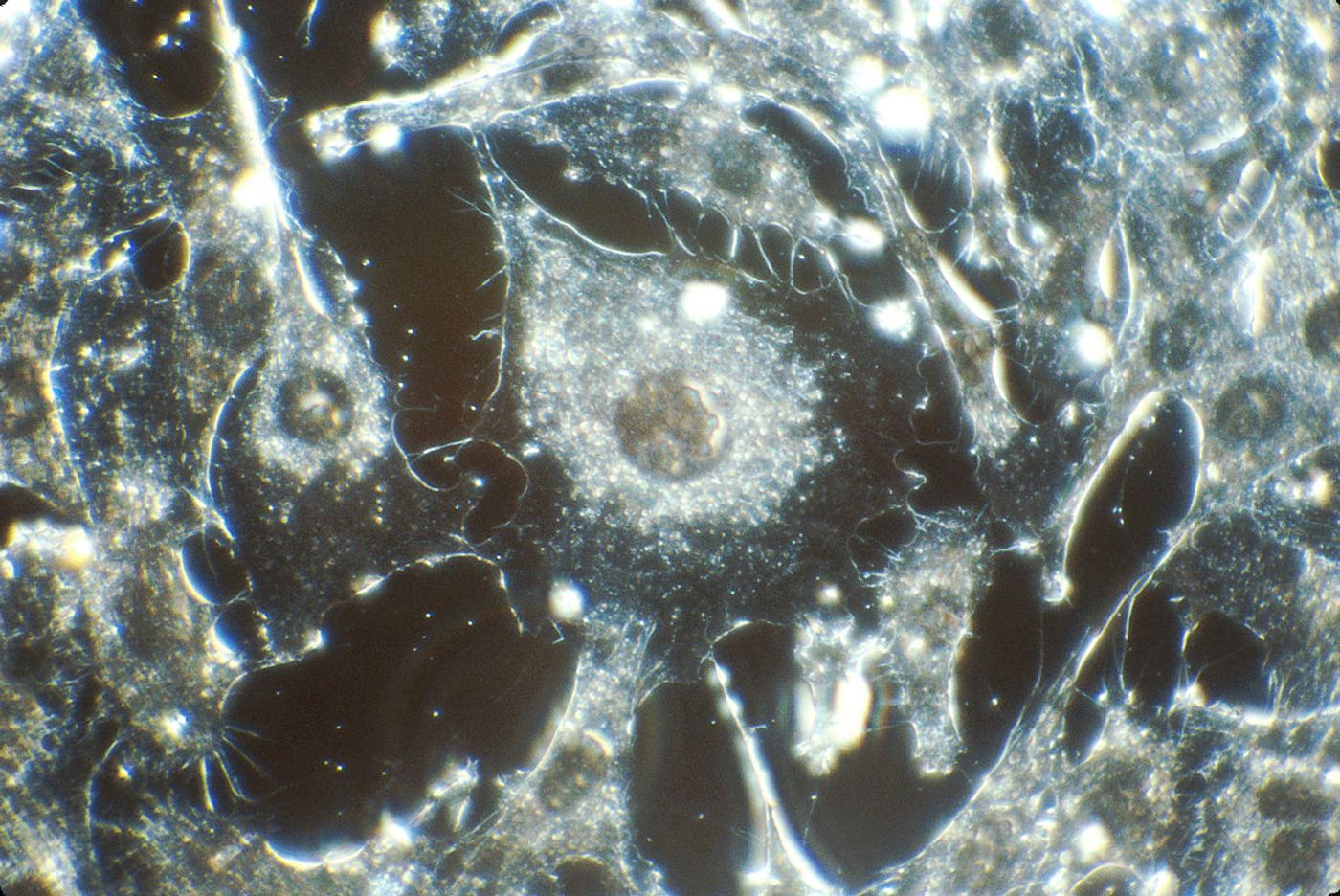
Cancer cells “learned” to manipulate the immune system’s set-in-place mechanism for keeping the inflammatory response in check by producing a cytokine called transforming growth factor-beta, or TGF-beta. Releasing this cytokine promotes an influx of Tregs into the tumor microenvironment, where the cancer cells can multiply and spread in peace with the blind protection of Tregs in place.
While not forgetting that some level of Treg activity is important for the prevention of autoimmune diseases and chronic inflammation, researchers from the Medical University of South Carolina (MUSC) brainstormed ways to prevent cancer cells from recruiting Tregs for their own agenda of proliferating and spreading to different parts of the body. Their investigation led them to a protein called moesin, which controls both Treg function and TGF-beta levels and activity.
"Because moesin supports greater Treg production, we could design moesin inhibitors to halt or slow active TGF-beta signaling and slow down Treg conversion so that anti-tumor T cells can have a chance to see the cancer and eradicate it," explained the senior author of the new study, Zihai Li, MD, PhD.
Li and the other researchers did not need to hinder Treg activity indefinitely, just long enough for fighter immune cells to identify abnormally growing cells as cancerous and launch an attack against them. What does this discovery mean? Maybe a new target for cancer immunotherapy.
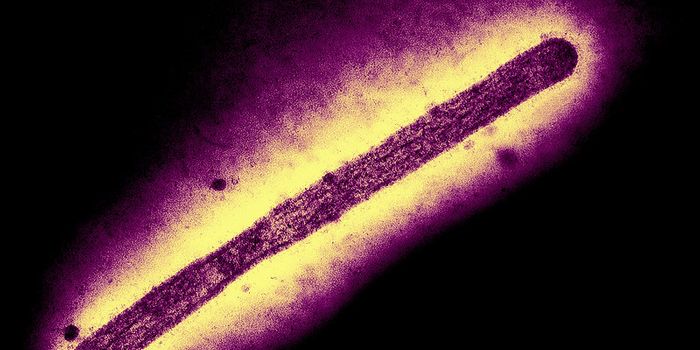
They applied their idea in a mouse model of melanoma alongside an existing experimental treatment called adopted T cell therapy. This approach involves taking fighter T cells from a cancer patient, “supercharging” them in the lab, and returning them to the patient with the intent of empowering the cells to better fight the cancer. The therapy is effective, but the supercharged cells do not live very long.
However, applying the adopted T cell therapy in models lacking moesin helped the superchargers live longer, fight cancer longer in the body. “We were not only deleting moesin but, when we gave T cells to the active tumors, those T cells could control the cancer for a very long time," explained lead author Ephraim Ansa-Addo, PhD.
Cancer remains an elusive and diverse disease with various subtypes that must be treated as individual diseases, but the new study from MUSC offers a new drug target that can be used alongside other treatments, boosting their effectiveness and long-term success.
The present study was published in the Journal of Clinical Investigation.