Atypical Form of Chronic Fatigue Stumps Researchers
It is uncertain what precisely causes myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), but it is definitely more than just excessive exhaustion. Now in a new study, researchers uncover that the disease is split into two forms, which follow different paths in the body to cause disease.
According to the ME Association, ME/CFS in all forms causes severe fatigue, muscle and joint pain, disordered sleep, gastric disturbances, and poor memory and concentration. While many of the details are unknown concerning this condition’s origin, scientists from Columbia University have identified two distinct forms of ME/CFS that differ based on immune signatures: classical and atypical.
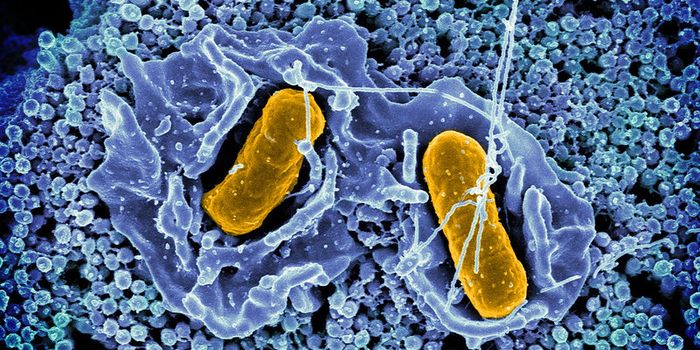
An immune signature consists of specific immune chemicals, often cytokines and chemokines, involved in a certain immune response. Like the immune signatures seen in a Strep throat infection would be different from a case of the flu, the two recently discovered forms of ME/CFS show different levels of immune molecules in the immune response.
These two “types” of ME/CFS also differ based on symptoms that characterize the beginning of the disease. Classical forms of the condition begin with a sudden, flu-like infection, but symptoms in atypical ME/CFS seem to come months or even years after the initial event that “triggers” disease.
Before the present study, researchers studying ME/CFS knew that the disease unfolded in distinct stages, including a major drop in immune molecules after the three-year mark of a person’s disease, making the immune signatures between people in early stages and people in later stages vastly different.
However, in the new study, while researchers saw a similar drop in the levels of immune molecules after the three-year mark, it was only in the study participants with classical ME/CFS; cases of atypical ME/CFS showed immune molecule levels stay the same or even increase after three years.
The study consisted of various immunoassays, biological experiments capable of measuring the immune molecules in a particular immune signature. In total they analyzed 51 immune biomarkers in cerebrospinal fluid samples, 32 cases of classical and 27 cases of atypical ME/CFS
Overall, they saw lower levels of immune molecules in individuals with atypical ME/CFS than those with the classical form of the disease. Specifically, they saw lower levels of a cytokine called interleukin-7 which is linked to viral infections, interleukin-17A, and chemokine (CXC motif) ligand 9 (CXCL9), which is an inflammatory molecule linked to neurological disorders.
Understanding the immunological differences between these two forms of the disease at a molecular level could help doctors understand a patient’s specific disease characteristics immediately following ME/CFS diagnosis as opposed to three years down the line, which could improve treatment options and long-term quality of life.
"Early identification of patients who meet the usual clinical criteria when first diagnosed but then go on to develop atypical features would help clinicians like myself identify and treat these complex cases and even prevent fatal outcomes," explained co-author Daniel L. Peterson, MD.
"Multiple biological pathways are likely involved in the pathogenesis of ME/CFS, with a range of clinical subtypes relating to variability in the types of environmental triggers, genetic and epigenetic vulnerability, as well as comorbidity patterns," said senior author Ian Lipkin, MD. "Shedding light on these pathways may help us to identify the various agents that precipitate disease as well as to design more precise, targeted treatments."
Researchers are still considering many more factors that might play a role in the deviated path taken by cases of atypical ME/CFS compared to the classical form of the disease: genetic susceptibilities, unidentified immune molecules that are involved, and cognitive dysfunction are all being considered.
The present study was published in the journal Translational Psychiatry.
Sources: ME Association, Immunity, Columbia University's Mailman School of Public Health