Immune Cells Patch Up Holes in the Gut
Immune cells are capable of making repairs in an intestine damaged by inflammatory bowel diseases. Either by boosting the activity of these cells or mimicking their reparative mechanisms, researchers believe they can develop a new treatment for those afflicted.
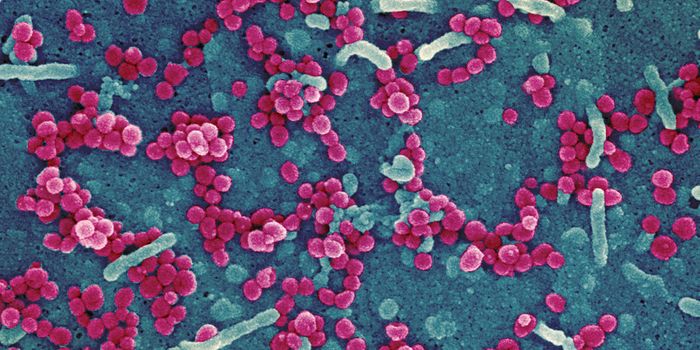
Inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis, is generally characterized by a disruption of the integrity of the intestinal epithelial barrier, a layer of tissue that prevents things traveling through the gut from reaching the rest of the body. Bacteria enter the intestine, breeze through the barrier, and trigger an immune response, causing excessive inflammation indicative of inflammatory bowel disease.
Thus, repairing the epithelial barrier is vital for healing the intestines and ridding the body of this disease. From Georgia State University, researchers found that immune cells called macrophages can produce interleukin 10 (IL-10), which works as a healing factor in the context of inflammatory bowel disease. IL-10 works its magic by interacting with receptors on intestinal epithelial cells to promote wound healing.
“We tried to understand some of the cellular mechanisms that are required for optimal wound healing in the intestine,” explained Dr. Dim Denning. “To do this, we used a cutting-edge system, a colonoscope with biopsy forceps, to create a wound in mice.”
Denning’s system used in mice mimics colonoscopies commonly conducted in humans. “This cutting-edge system allowed us to begin to define what cells and factors contribute to wound healing in the mouse model,” Denning said.
Specifically, Denning and his team compared normal (wild-type) mice with mice genetically deficient in IL-10, particularly the macrophages, looking at the ability of each group to repair epithelial wounds. Without IL-10, the mice were largely inept at wound-healing in the intestines.
Based on this finding, Denning believes that there is potential for new therapeutic interventions for people with inflammatory bowel disease.
"There are different ways we think about it, but perhaps we could deliver the beneficial compounds (IL-10 and the downstream signaling pathways) to those patients, orally or even intravenously, or somehow drive the natural production of those compounds,” he said.
The present study was published in The Journal of Clinical Investigation.
Sources: Georgia State University