Is Stress Making You Sick?
Increased stress - either psychological or allergic - can make the body’s response to disease much more serious. In a new study from Michigan State University, scientists investigate the impact of stress-induced disease when the body lacks a certain immune cell receptor.
"This work is a critical step forward in decoding how stress makes us sick and provides a new target pathway in the mast cell for therapies to improve the quality of life of people suffering from common stress-related diseases,” explained Michigan State’s Adam Moeser.
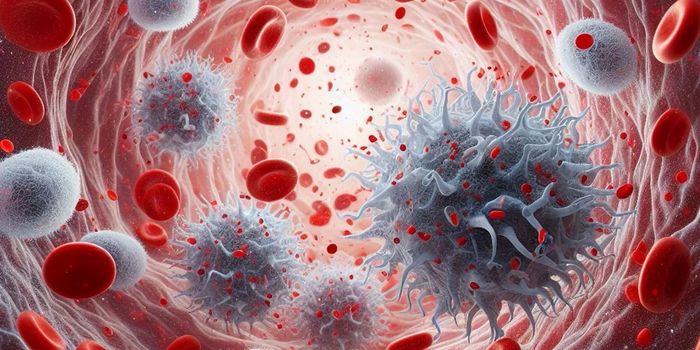
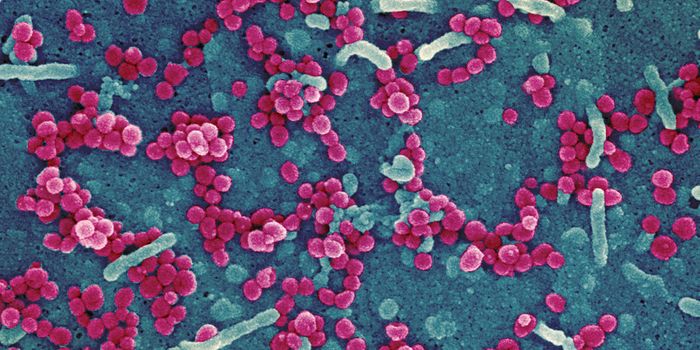
Mast cells are immune cells involved in both in the innate, or non-specific, and adaptive, or specific, immune response. Additionally, past research has linked them with dilation of blood vessels, creation of new blood vessels, and venom detoxification.
Moeser’s new study involves a stress receptor called corticotropin-releasing factor (CRF1). In response to stress, CRF-1 releases corticotropin, a polypeptide hormone. Ultimately, CRF1 sends signals to mast cells and influences their activity.
“CRF1 tells [mast] cells to release chemical substances that can lead to inflammatory and allergic diseases such as irritable bowel syndrome, asthma, life-threatening food allergies and autoimmune disorders such as lupus,” Moeser said.
The new study tested the histamine response of mice to either psychological stress or allergic stress. Histamine is a compound produced by the body to eliminate allergens like pollen or food proteins. Histamine is present in both normal allergic reactions like sneezing and in more serious reactions that can result from excess stress or a severe allergy. In the case of more serious allergic reaction, sneezing can become trouble breathing, anaphylactic shock, or death.
Researchers tested the response of histamine to stress with two different groups of mice: those with CRF1 receptors intact, and those with mast cells lacking the receptors. For the mice lacking CRF1 receptors, results showed low levels of histamine, a 54 percent reduction in disease when exposed to allergic stress, and a 63 percent disease reduction after exposure to psychological stress.
"This tells us that CRF1 is critically involved in some diseases initiated by these stressors,” Moeser said.
Moser and the rest of the research team hope to apply their new understanding of the relationship between CRF1, mast cells, the histamine response, and allergic reactions to the clinic. Potentially, the could one day identify new ways to treat troublesome allergic diseases such as asthma and irritable bowel syndrome.
The present study was published in the Journal of Leukocyte Biology.
Sources: Michigan State University, Gene ID, DrugBank, News Medical Life Sciences, Frontiers in Immunology