Sugar Disrupts the Microbiome, Altering Immunity
The microbes in our gut are indispensable to our health, and they are affected by what we eat. New research has used a mouse model to show that sugar intake can change the composition of the gut microbiome, which has a cascade of effects that can ultimately cause weight gain, pre-diabetes, and metabolic disease. This study has shown that diet and the microbiome are both related to the prevention of metabolic disease and obesity. The findings have been reported in Cell.
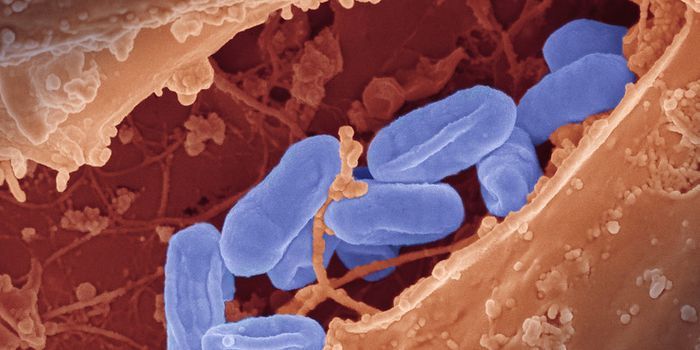
A Western-style diet, which is high in sugars and fats, is known to increase the risk of obesity, metabolic disorders, and diabetes. When mice were put on such a diet for four weeks, they gained weight, showed signs of insulin resistance, and metabolic disease. The composition of their microbiomes also changed significantly. The levels of segmented filamentous bacteria, which are commonly found in rodent, fish, and chicken gut microbiomes, dropped, while the levels of other microbes increased.
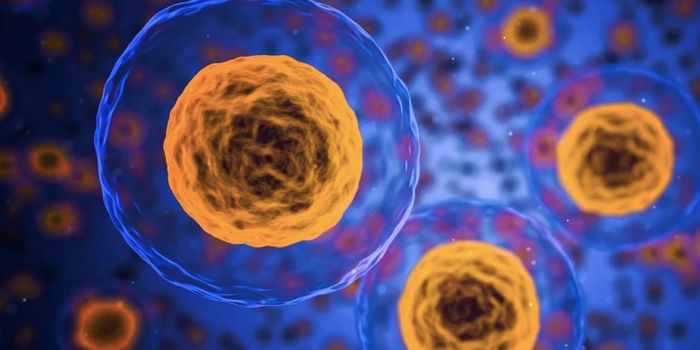
As the number of filamentous bacteria dropped, the amount of immune cells called Th17 cells was also reduced. Those Th17 cells appear to be critical to the prevention of metabolic disease, weight gain, and diabetes.
"These immune cells produce molecules that slow down the absorption of bad lipids from the intestines and they decrease intestinal inflammation," noted Ivalyo Ivanov, Ph.D., an associate professor at Columbia University Vagelos College of Physicians and Surgeons. "In other words, they keep the gut healthy and protect the body from absorbing pathogenic lipids."
The researchers determined that sugar was to blame for the elimination of filamentous bacteria. Once those microbes are gone, the consequence is that protective Th17 cells also disappear, said Ivanov.
When mice were fed a diet that was rich in fats but low in sugar, the Th17 cells were maintained in the intestine, and the mice did not get obese or develop pre-diabetes, even though they consumed the same number of calories, added Ivanov.
Not all mice benefited from the elimination of sugar, however. If mice did not have any filamentous bacteria to begin with, the animals became obese and diabetic when fed a diet high in fats but lacking sugar.
"This suggests that some popular dietary interventions, such as minimizing sugars, may only work in people who have certain bacterial populations within their microbiota," Ivanov said.
Some probiotics could be useful in such a situation. When the mouse model received supplements of filamentous bacteria, Th17 cells recovered and the mice were once again protected from the adverse impacts of a high fat diet.
People do not carry the same filamentous bacteria as rodents, but Ivanov suggested that these findings may still hold true for us. More research will be needed to confirm that hypothesis.