A new cell-based model of the human placenta could help explain how pathogens cross from mother to unborn child.
The researchers are beginning to use their model to test whether Zika virus, and other pathogens associated with congenital disease, can infect placental cells and/or cross the placental barrier.
“The human placenta is unique and unlike that of other many other placental mammals,” says Carolyn Coyne, ssociate professor of microbiology and molecular genetics at the University of Pittsburgh School of Medicine. “With our new model in the research toolkit, we and other scientists hope to advance our knowledge of the placenta, examine its function, and learn how it can prevent most, but not all, maternal infections from causing problems for the baby.”
Researchers currently can obtain and study placental cell lines, but such cells do not fuse spontaneously to form the characteristic structure of the human organ. Some scientists study cells, called primary human trophoblasts, that are isolated from placentas obtained after childbirth, but such cells do not divide, can be more difficult to obtain, and are more difficult to genetically manipulate to learn about biochemical pathways that have a role in placental function, says Coyne, senior investigator of the study published in
Science Advances.
A different approach
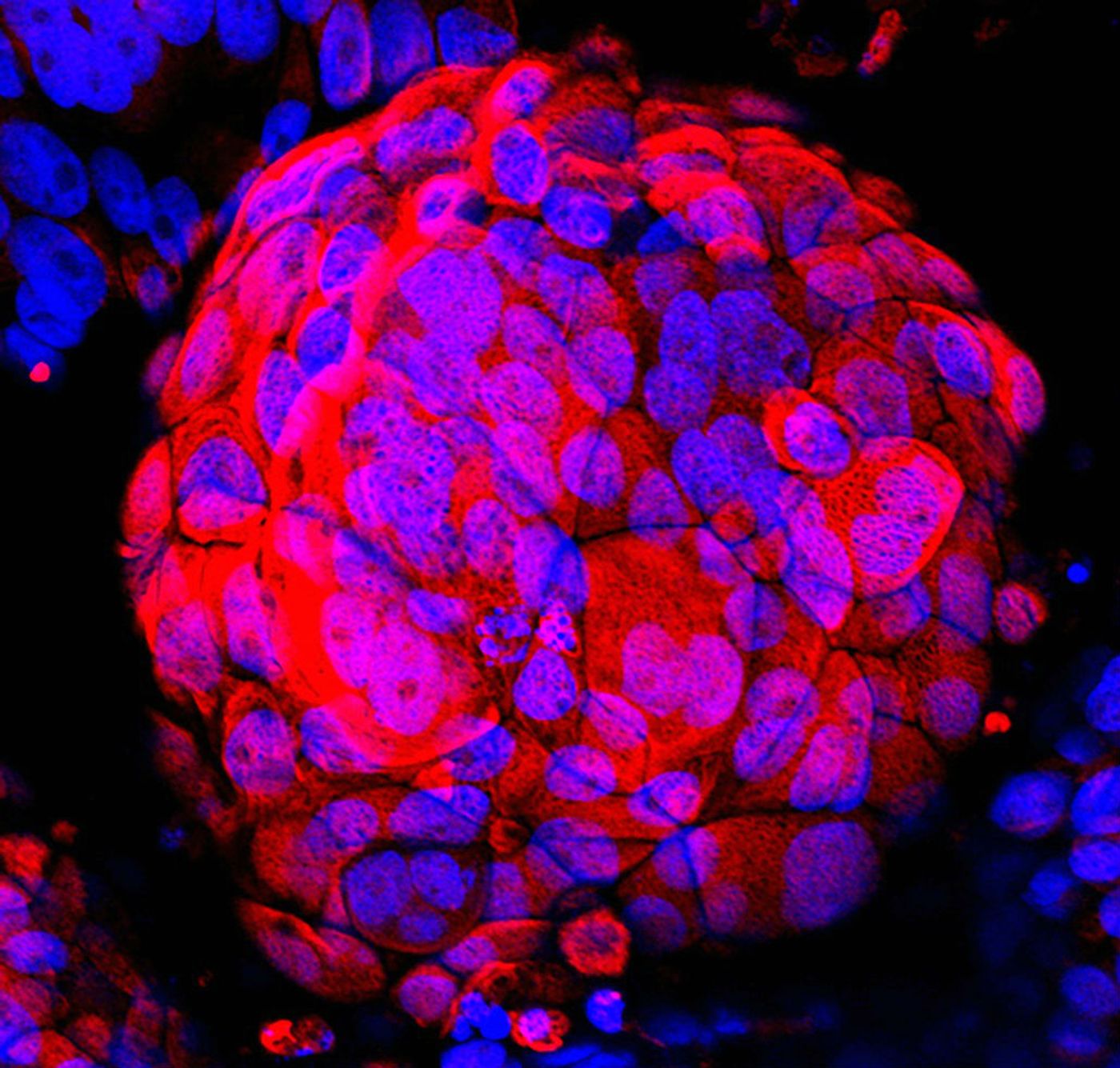
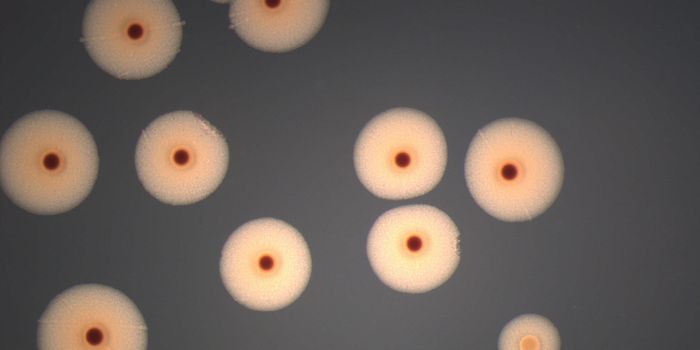
Coyne’s team cultured a human placental trophoblast cell line in a microgravity bioreactor system developed by NASA. The trophoblasts along with blood vessel cells were added to small dextran beads that were then spun around in a container filled with cell culture fluid, creating shear stress and rotational forces to better mimic the environment at the maternal-fetal interface than static cell-culture systems.
As a result, the cells fused to form syncytiotrophoblasts, and thus more closely resemble the primary cells lining the outermost layer of the tree-like or villous structure of the human placental tissue.
Next, the researchers tested the functional properties of their model by exposing it to a virus and to Toxoplasma gondii, a parasite found in cat feces that can lead to fetal infection, causing miscarriage, congenital disease, and/or disability later in life.
“We found that the syncytiotrophoblasts formed in our system recapitulated the barrier properties of the naturally occurring cells and they resisted infection by a model virus and three genetically different strains of Toxoplasma,” says Jon P. Boyle, co-investigator and associate professor of biological sciences. “With this model, we can experiment with different biological factors to see what might allow an infectious agent to get through the placental barrier to the fetus.”
He says understanding the placenta might one day lead to ways to prevent fetal damage from the so-called TORCH infections: toxoplasmosis, rubella, cytomegalovirus, herpes, and HIV.
Additional researchers from the University of Pittsburgh, Arizona State University, and Johns Hopkins University contributed to the research, which was funded by the National Institutes of Health and the Burroughs Wellcome Fund.
Source: University of Pittsburgh
This article was originally posted on
futurity.org.