Recent research at the Johns Hopkins University School of Medicine may have found a new blood biomarker for episodic migraines. The new study, which only looked at women, discovered levels of a group of lipids called ceramides that decreased with episodic migraines as compared to those without any headaches.

Each standard deviation increase in total ceramide levels was associated with more than a 92-percent lower risk of having migraines. The lipids help to regulate inflammation in the brain. The findings were published online September 9 in the journal Neurology and reported by Bevin Fletcher in
Bioscience Technology.
According to study author B. Lee Peterlin, DO, Johns Hopkins, “While more research is needed to confirm these initial findings, the possibility of discovering a new biomarker for migraine is exciting.”
He explained, “Study participants gave blood samples, underwent a neurological exam and had their body mass (BMI) measured. The study looked at 36 women who did not have headaches, and 52 women with episodic migraines, which is defined as having less than 15 headaches per month. On average the women with migraines had 5.6 headaches per month.”
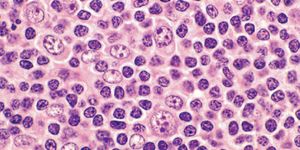
The blood tests indicated that women without headaches had about 10,500 nanograms per milliliter of total ceramides in their blood, as compared with women with migraines, who had about 6,000 nanograms per milliliter. The researchers also tested two other types of lipids, called sphingomyelin, and each standard deviation increase in their levels was associated with a 2.5 times greater risk of migraine.
When testing the blood of a random small sample of 14 participants, the researchers could accurately determine migraine suffers or controls without headaches based on these blood lipid levels. The researchers said that there are limitations in the study, including chronic migraines not being included, and that a large number of participants had migraine with aura (a perceptual disturbance that sometimes precedes migraines).
According to the
National Institute for Neurological Disorders and Stroke, people describe the pain of a migraine headache as an intense pulsing or throbbing pain in one area of the head. The International Headache Society diagnoses a migraine by its pain and number of attacks (at least five, lasting 4 to 72 hours if untreated), and additional symptoms including nausea and/or vomiting, or sensitivity to light and sound. Three times more common in women than in men, migraine affects more than 10 percent of people worldwide. About one-third of affected individuals can predict the onset of a migraine, which is preceded by an "aura," visual disturbances that appear as flashing lights, zig-zag lines or a temporary loss of vision. People with migraine tend to have recurring attacks triggered by a number of different factors, including stress, anxiety, hormonal changes, bright or flashing lights, lack of food or sleep, and dietary substances. Migraine in some women may relate to changes in hormones and hormonal levels during their menstrual cycle. While scientists used to link migraines to the dilation and constriction of blood vessels in the head, they now suspect a genetic cause.