Exploiting a Cell's Love of Zinc to Deliver Targeted Therapeutics
Diabetes is a growing problem around the world, and while careful monitoring and control of insulin levels can help people manage the disease, scientists are looking for better ways to treat and potentially cure the disorder. Years of research have taught us that the pancreas carries beta cells, which produce the hormone insulin. One of the hallmarks of type 2 diabetes is the death of those insulin-producing beta cells, which exacerbates the disease. Regenerating them is a potential way to cure the disease.
That, of course, is easier said than done. Regenerative treatments are usually applied in a way that affects cells throughout the whole body, which could potentially cause many other problems. A regenerative therapy for diabetes would mean selectively growing only new beta cells. A team of researchers at Stanford University may have found a way towards that type of targeted therapy.
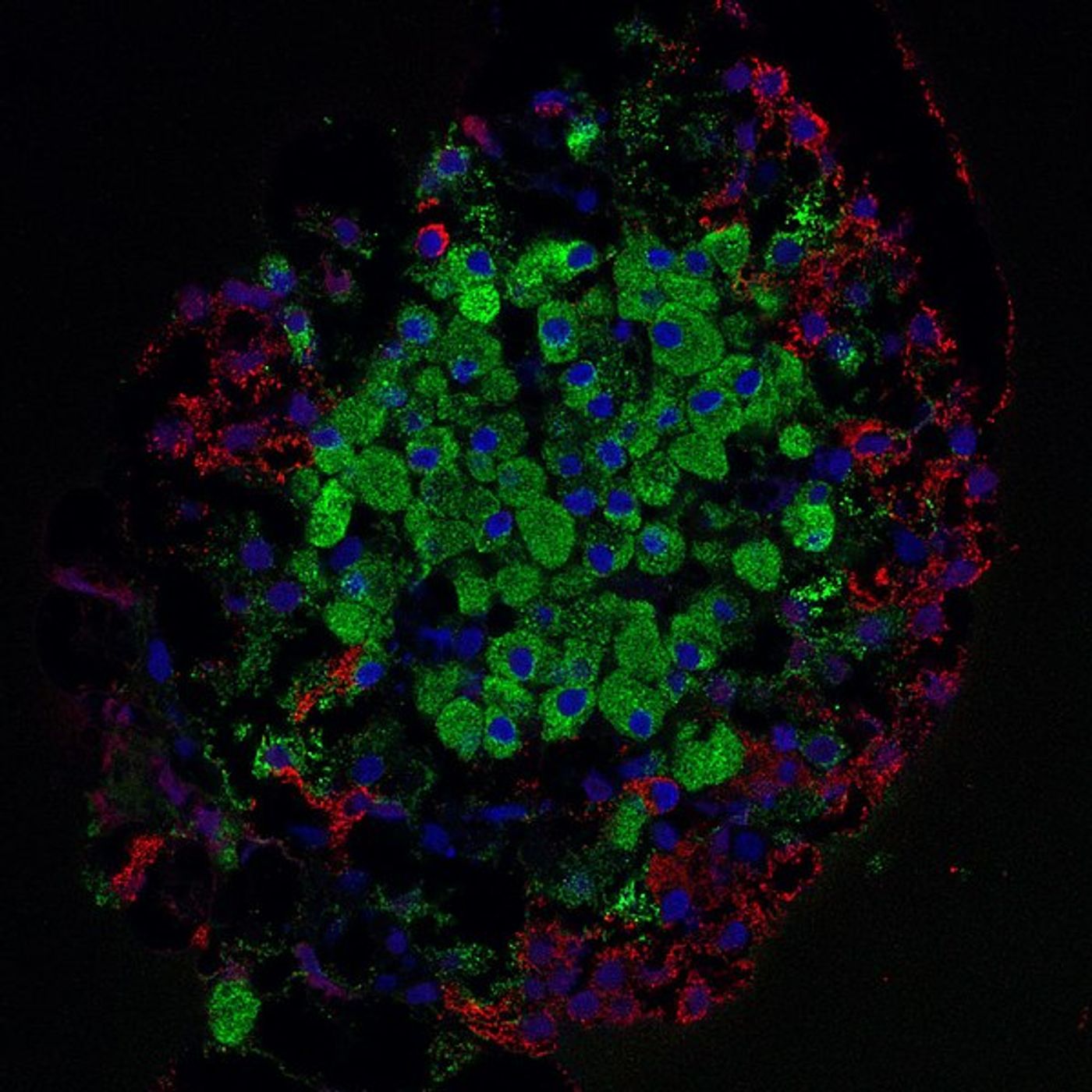
It was established decades ago that beta cells love to take in zinc. While that has been exploited for research purposes and made it easy for scientists to visualize beta cells in pancreatic samples, Justin Annes, MD, Ph.D., assistant professor of medicine, wanted to see if zinc could be used as a way to transport therapeutics directly to beta cells.
"The only problem was, I didn't know how to generate compounds that could test this hypothesis," Annes said. He brought chemistry graduate student Timothy Horton and Stanford ChEM-H senior research scientist Mark Smith, director of the Medicinal Chemistry Knowledge Center, onto the project.
The team used an approach based on chelation, in which a drug tightly bonds with a chemical, which is usually used to rid the body of poisonous metals like lead and mercury. In this strategy, the aim is to bond a zinc-chelating agent to any zinc it encounters and then deliver it to zinc-lovers like beta cells.
This work, which was reported in Cell Chemical Biology, is nowhere near ready for patients, but it presents a totally new approach to dealing with diabetes. "We're at the earliest stages," Annes said.
An initial test of their hypothesis showed that when a beta-cell regenerating drug was attached to a zinc-chelating agent, the drug ends up in beta cells growing in a lab dish.
The researchers also demonstrated that the drug wasn’t just getting into any cell; it was accumulating in beta cells more than any other cell type. When a dish of rat cells, including beta cells, were exposed to the drug, the beta cells regenerated around 250 percent more than other types of cells. When the same treatment was given to human cells, beta cells regenerated roughly 130 percent more than others.
It’s too early to get excited about using this drug as a diabetes cure, but it shows that it’s an idea worth pursuing. "This is the first demonstration of a selectively delivered replication molecule in beta cells," Annes added, and "it's not sufficient for therapeutic applications." The selectivity shown in the experiments has given the researchers reason to continue the work.
Recent research has indicated that insulin is becoming more expensive and may become much harder for diabetics to obtain in the future; it makes work that could eliminate the need for insulin all the more pressing. The video below from NBC News features a story on Americans who are rationing their insulin because they cannot afford to buy what they need.
Sources: AAAS/Eurekalert! via Stanford Medicine, JAMA, Cell Chemical Biology