Focusing on the Cause of Neurological Symptoms of COVID-19
We now know that COVID-19 can cause a range of problems in the brain. Some of these problems are taking months to clear up in patients, or they are still lingering. They may be on the milder side, like disruptions in the ability to sense smells or tastes, or they may be far more severe, with some patients complaining of memory problems and brain fog. Researchers have been trying to learn exactly how these symptoms are arising; for example, is the virus infecting the brain directly? Or is the brain impacted in a secondary way?
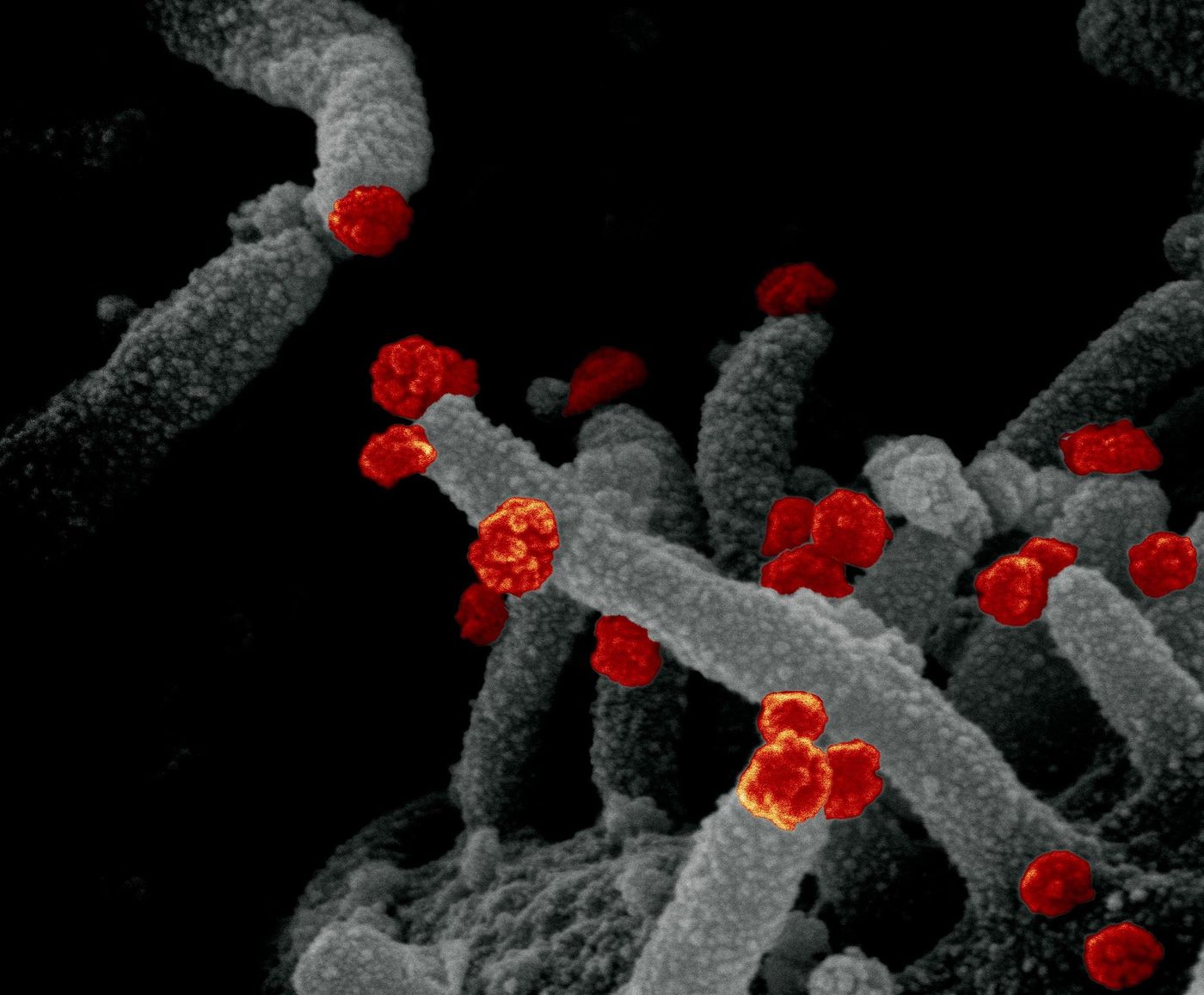
The blood-brain barrier seems to do a pretty good job of protecting the brain from the SARS-CoV-2 virus; viral levels seem to be very low in infected individuals. However, the virus can get into cells that make up the olfactory epithelium, a border that lines the nasal cavity and is also very close to the brain. The virus may be able to infect cells in the brain called astrocytes, which have a variety of roles. Astrocytes were once thought to work primarily to support neurons, but research has indicated that have other functions as well.
A recent preprint, not yet peer-reviewed, has suggested that SARS-CoV-2 can infect astrocytes in brain organoids, which are small, miniature models of human brains. Preliminary work by researchers in Brazil proposed that five people out of a group of 26 who had died from COVID-19 had evidence of SARS-CoV-2 infection in their brain cells; 66 percent of the infected cells in these patients were astrocytes. Another report compared gene expression in patients that had died of SARS-CoV-2 to controls, and determined that gene expression in astrocytes was disrupted even though the virus was not found there.
There may be no simple answer to the question of how many brain cells have to be infected for a problem to occur, Arnold Kriegstein, a neurologist at the University of California, San Francisco and a co-author on the organoid study told Nature. He explained that damaged cells in some regions of the brain might cause more problems than others.
There may also be another way that the virus causes neurological symptoms. Since the early days of the pandemic, clinicians and researchers noticed unusual blood clots in patients. Blood flow to the brain might be disrupted in some COVID-19 patients. Capillaries, which are vessels that move blood to small places in the body, also contain a type of cell called pericytes. According to a pre-print, SARS-CoV-2 can infect pericytes, and pericyte-like brain cells.
Another possibility is that the immune system overreaction induced by COVID-19 is also battering the brain. Some people generate autoantibodies, which attack their own cells, during the course of a serious infection. There is evidence that suggests these autoantibodies can pass through the blood brain barrier and play a role in neurodegenerative disorders.
Researchers are now working to earn more about autoantibodies in COVID-19 patients. One study has found that eleven of these critically ill patients all carried autoantibodies that could attach to neurons.
Treating these problems may be very complicated; clinicians might have to determine which mechanism is most likely causing a patient's problems, or researchers may have to focus on creating a treatment that targets the one that's most common.
Sources: Journal of Neurology, Neurosurgery, and Psychiatry, Nature