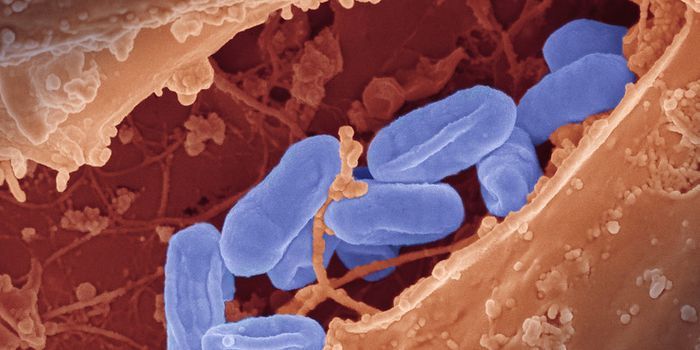
Clostridium difficile is most commonly referred to as a healthcare-associated infection (HAI), with at risk-populations including older adults who are currently receiving medical care or who are taking antibiotics. According to the CDC, in 2011 there were approximately 50,000 infections caused by C. difficile. Of the persons infected 29,000 died within 30 days of their initial diagnosis. C. difficile is a type of spore-forming bacteria that produces two types of enterotoxins. It accounts for 15-25 % antibiotic associated diarrhea (AAD). C. difficile infection can also result in pseudomembranous colitis (PMC), toxic megacolon, perforations of the colon, sepsis and sometimes death. It is currently regarded as the leading cause of hospital-acquired infections in the US.

Researchers at the University Of Maryland School Of Medicine have recently discovered that certain species present in the gut may help protect colonization by C. difficile. When the normal microflora in the gut are wiped out by antibiotics, C. difficile has the opportunity to colonize the gut and produce enterotoxins, which is why antibiotic treatment is considered a major risk factor for acquiring a C. difficile infection. In their study, researchers administered one of 7 different antibiotics in mice order to alter the indigenous bacteria present in the gut. Following a 24 h recovery period, mice were challenged with C. difficile spores. Fecal samples from the treated mice were collected on the day of the C. difficile challenge as well as the day after the challenge. Fecal samples were processed to enumerate aerobic as well as anaerobic bacteria present in the samples followed by DNA sequencing. The research team used relative abundance data to build a machine learning regression model to predict the levels of C. difficile that could be found in the fecal samples 24 h following the challenge.
Bacterial populations including Porphyromonadaceae, Lachnospiraceae, Lactobacillus, and Alistipes were reported to be protective against C. difficile colonization and Escherichia and Streptococcus species were found to help enhance C. difficile colonization. One species, Akkermansia, was found to have a strong dependency on other members of the microbiota. The authors of the study concluded that individual bacterial populations do not drive colonization resistance to C. difficile. Instead, authors believe that different bacterial species present in the gut work together to mediate colonization resistance against C. difficile.
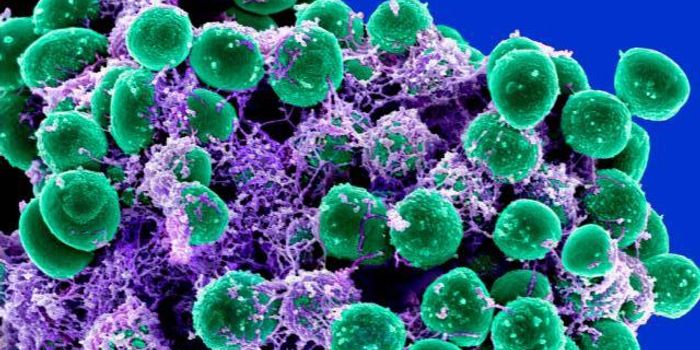
The findings of this study could lead to better methods to assess the risk of a particular patient to acquire a hospital acquired infection, such as C. difficile. This would require sequencing of the patient's gut microbiota to determine what bacterial species are missing and added back via probiotic treatment. This method could be used as a pre-screening preventative, similar to those used to screen for MRSA in hospital settings upon admission of a new patient.
Sources: CDC, American Society for Microbiology