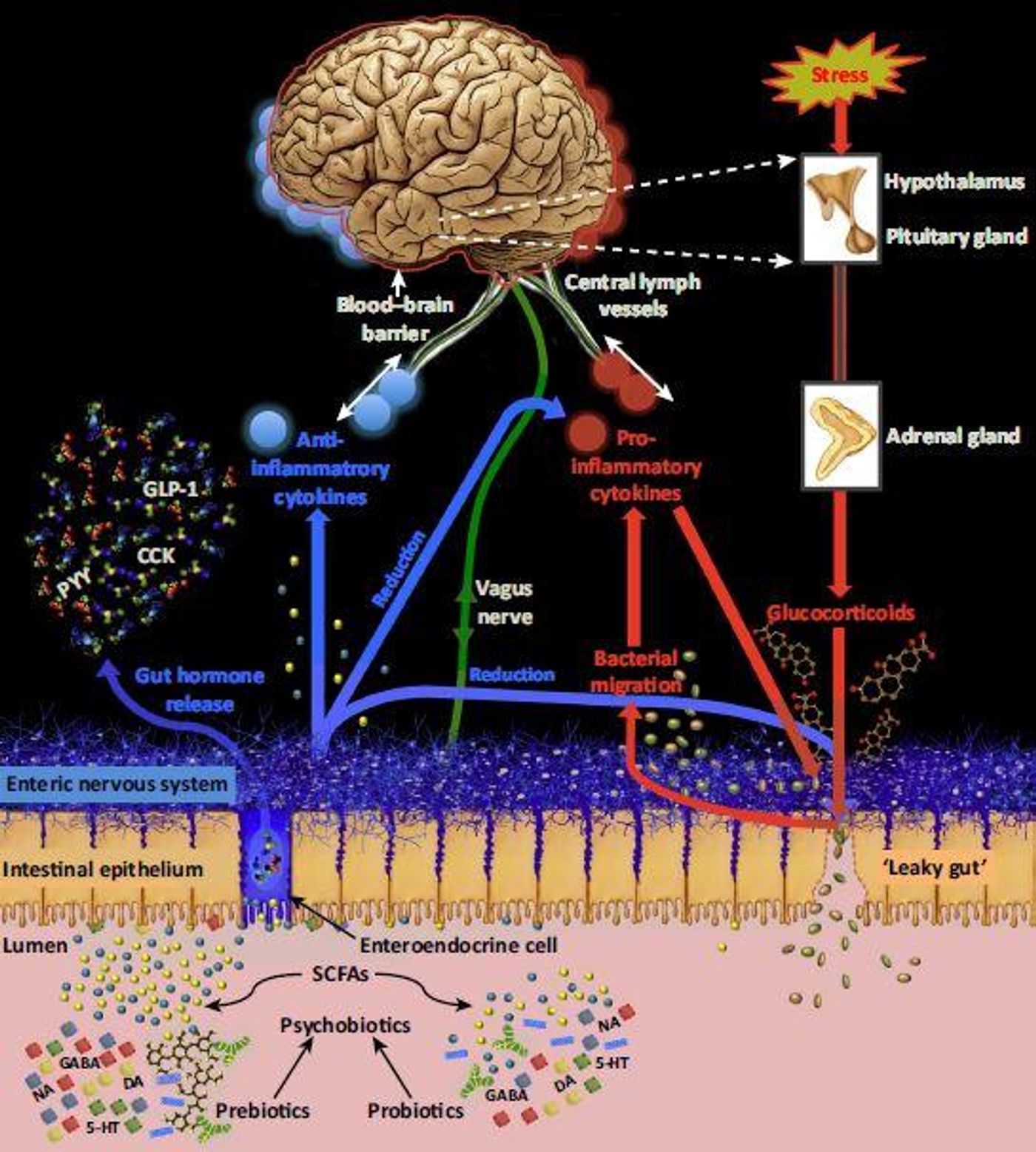
Researchers have known for some time that the myriad bacteria that reside in our gut - our microbiome - can communicate with our brain, exerting an effect on things like our moods, appetites and our circadian rhythms. Very little is known however, about controlling that relationship. In the journal Trends in Neurosciences,
a new review discusses new ideas about exploiting bacteria to alter the brain, potentially providing mental health benefits, as well as the hurdles science has to confront before success can be achieved.
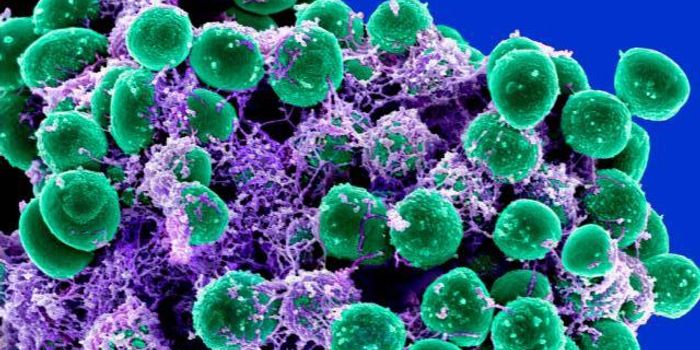
Psychobiotics is a relatively new term that describes organisms that produce a mental health benefit when sufficiently ingested by a patient with a psychiatric illness. The gut-brain connection has only begun to be studied in the past decade or so; after all, the microbiome itself has only recently been studied to an intensive degree.
Studies performed in mice have demonstrated improved response to stress, enhanced immune function, and memory and learning advantages, all conferred from the receipt of the proper strain of bacteria. Studies done with human subjects have been far more challenging to understand, not only because of the self-reporting that is common to the studies and small numbers of patients, but also because of physiological shifts in inflammation and reduced corticol levels.
"Those studies give us confidence that gut bacteria are playing a causal role in very important biological processes, which we can then hope to exploit with psychobiotics,”explained the lead author of the review, Philip Burnet, an Associate Professor of Psychiatry at the University of Oxford. "We're now on the search for mechanisms, mainly in animal models. The human studies are provocative and exciting, but ultimately, most have small sample sizes, so their replicability is difficult to estimate at present. As they say, we're 'cautiously optimistic.'"
It’s likely that the nervous system of the gut, the immune system, and vagus nerve are crucial parts of the bacteria-gut-brain-axis, potentially working with hormones and neurotransmitters like dopamine and serotonin. It remains to be seen, however, whether psychobiotics could be worthwhile therapies for psychological disorders, or if they could improve brain function. Studies have not yet conclusively indicated any mental health benefit from probiotic ingestion. Probiotics, however, aren’t the only players.
"Prebiotics (nutrition for gut bacteria) are another channel to alter gut bacteria," Burnet said. "We call for an even further widening of the definition of 'psychobiotics' to include drugs such as antidepressants and antipsychotics, and activities such as exercise and eating, because of their effects on gut bacteria."
Consumers should exercise a healthy degree of skepticism when evaluating any product that claims to have psychobiotic effects.
"Psychobiotics are a long way from their true translational potential. It's a little boring to say that we need more studies, but that is always the case in any academic discipline," Burnet commented. "The technology and resources already exist for such investigations, so though we are enthusiastic, the enthusiasm needs to be tempered and channeled toward answering the core mechanistic questions."
If you’d like to know more about psychobiotics, you can watch the video above from the National Human Genome Research Institute on the topic of Microbiome, Brain and Behavior, with Ted Dinan. Additionally, you can
view a lecture, here, presented by the NIH, “Towards Psychobiotics: The Microbiome as a Key Regulator of Brain and Behavior” with John Cryan of University College in Cork Ireland.
Sources:
AAAS/Euerkalert! via
Cell Press,
Biological Psychiatry,
Trends in Neurosciences